To the Editor,
The patent oval foramen (PFO) is present in nearly 1 out of every 4 people, and for the vast majority of them, it has no clinical implications.1 In others, however, it can trigger strokes, migraines or the orthostatic decompression or desaturation syndrome (known as platypnea-orthodeoxia syndrome).2 An even rarer presentation of PFO that can occur in the adult age is exercise-induced desaturation, which has been described in very few literature reviews and with a term not fully coined.3,4
This is the case of a 79-year-old woman with a past medical history of hypertension and diabetes referred to the cardiac rehabilitation unit due to dyspnea and poor functional capacity. The patient had previously undergone various tests including transthoracic echocardiography, pulmonary function tests, computed tomography pulmonary angiography, and coronary catheterization, all of which showed no significant findings. The physical examination revealed oxygen saturation levels around 98%, blood test results were normal, and N-terminal pro-brain natriuretic peptide levels, 255 pg/mL.
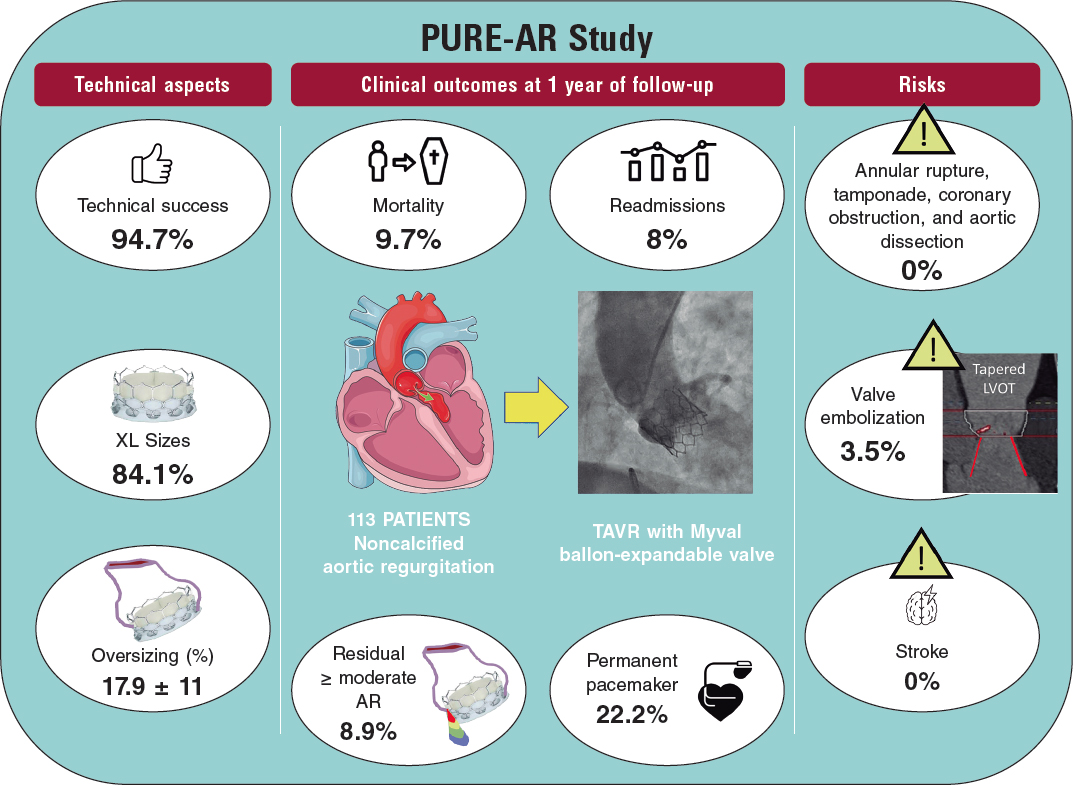
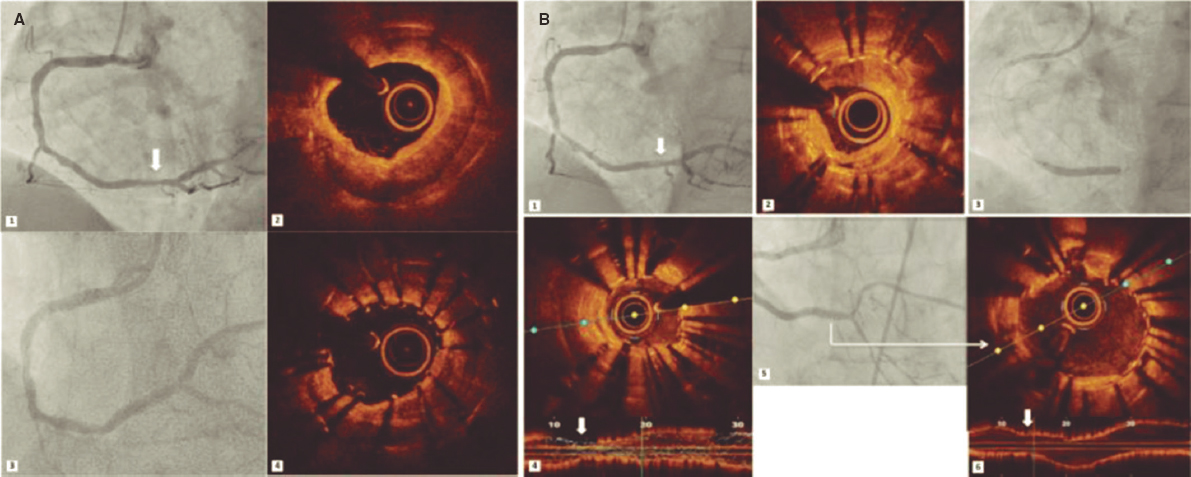
Atthe office, she complained of exertional dyspnea that had just appeared after walking from the waiting room to the office. Then, a pulse oximeter was placed on her, and she was told to go for a walk. Oxygen saturation progressively dropped down to 87%, and symptoms relapsed. However, they quickly normalized with rest even in an upright position. The treadmill exercise stress testing revealed the presence of significant saturation changes during exercise (values between 88% and 96%) followed by a sudden increase of ventilation, ventilatory equivalents (VE/VO2 and VE/VCO2), a quick drop of end-tidal carbon dioxide pressure (PETCO2), and a sudden increase of end-tidal oxygen pressure (PETO2) (figure 1A,C,E; Wasserman plots 1, 6, and 9, respectively).
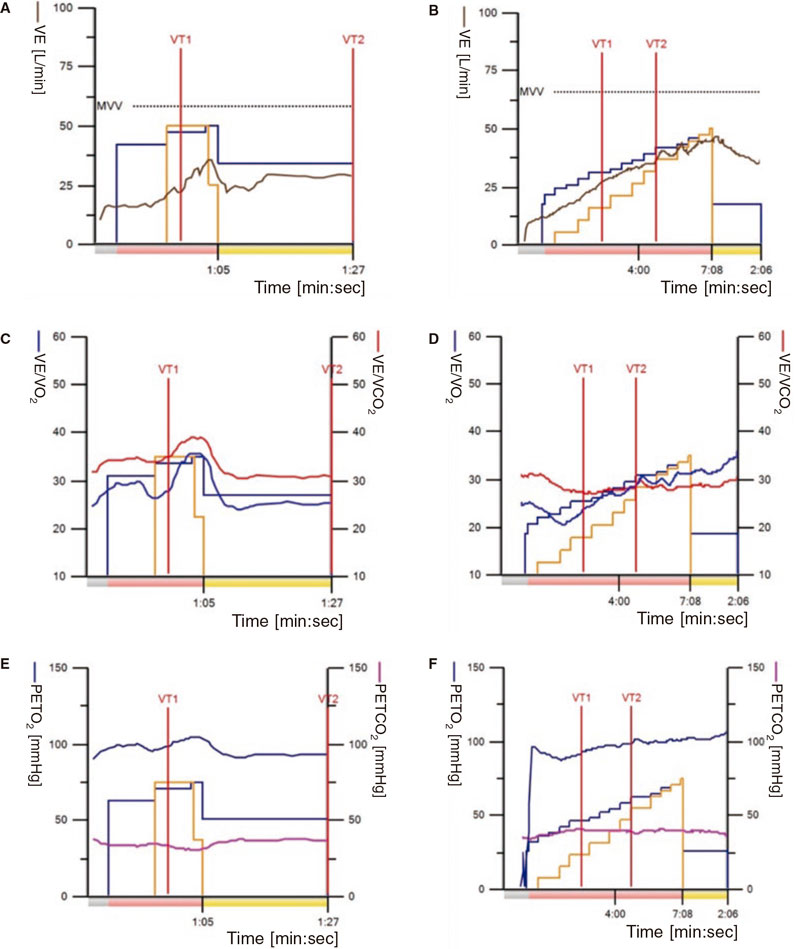
Figure 1. Comparison of multiple treadmill exercise stress testing performed at the cardiology unit. A, C, and E: test conducted before closing the foramen. B, D, and F: test conducted after closure with a device. PETCO2, end-tidal carbon dioxide pressure; PETO2, end-tidal oxygen pressure; VE/VCO2, ventilatory equivalent for carbon dioxide; VE/VO2, ventilatory equivalent for oxygen
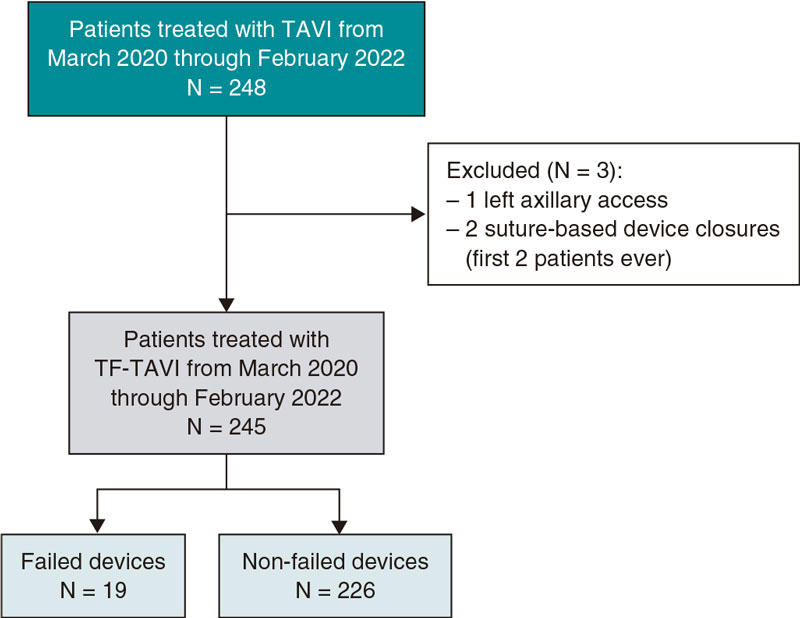
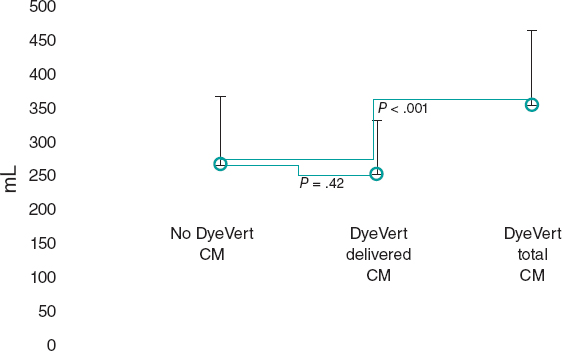
The presence of a shunt was suspected, and a transesophageal echocardiography was performed that revealed a large PFO (a 15 mm tunnel and a 3 mm to 5 mm separation) with bidirectional shunt whose right-to-left flow increased significantly with the Valsalva maneuver (figure 2 and video 1 of the supplementary data).
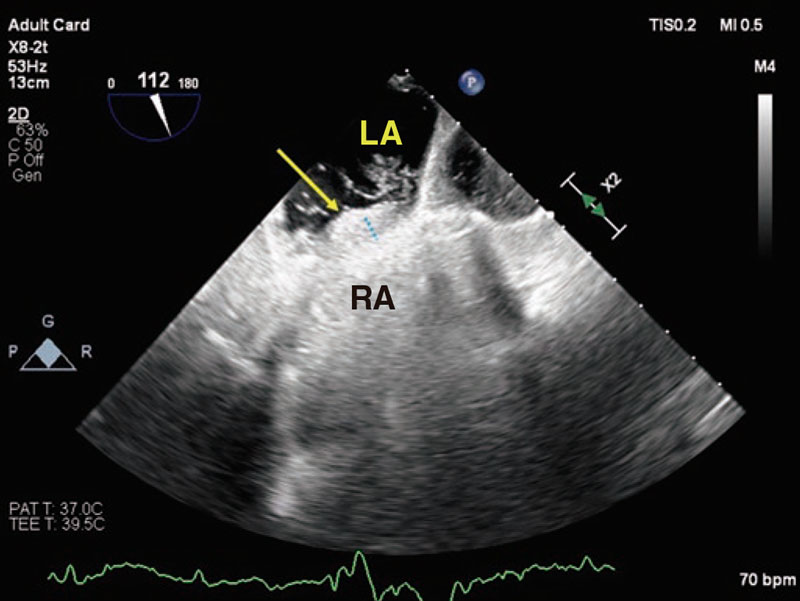
Figure 2. Transesophageal echocardiogram in a modified bicaval view to visualize the passage of bubbles through the tunnel made by the foramen (blue dotted line) from the right (RA) to the left atrium (LA). The yellow arrow indicates the ostium primum.
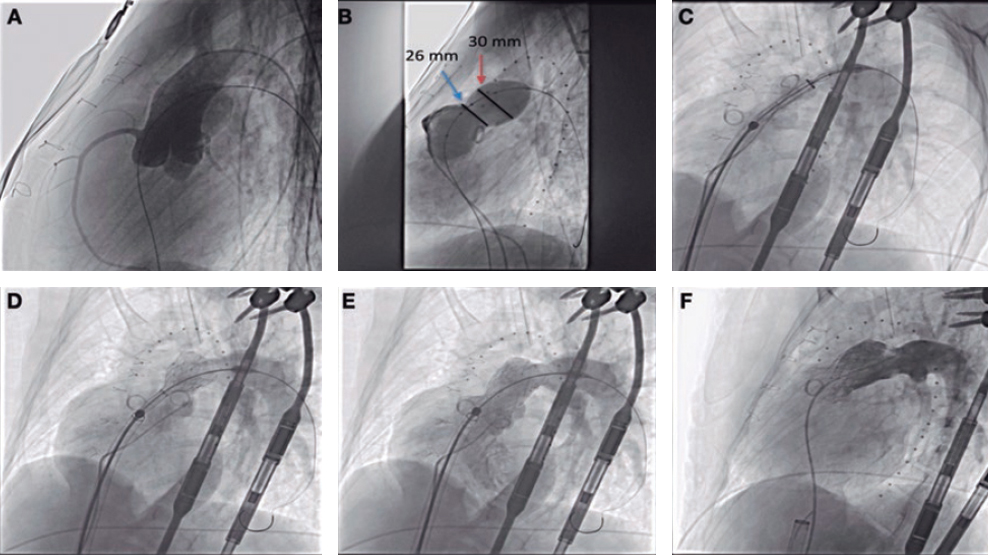
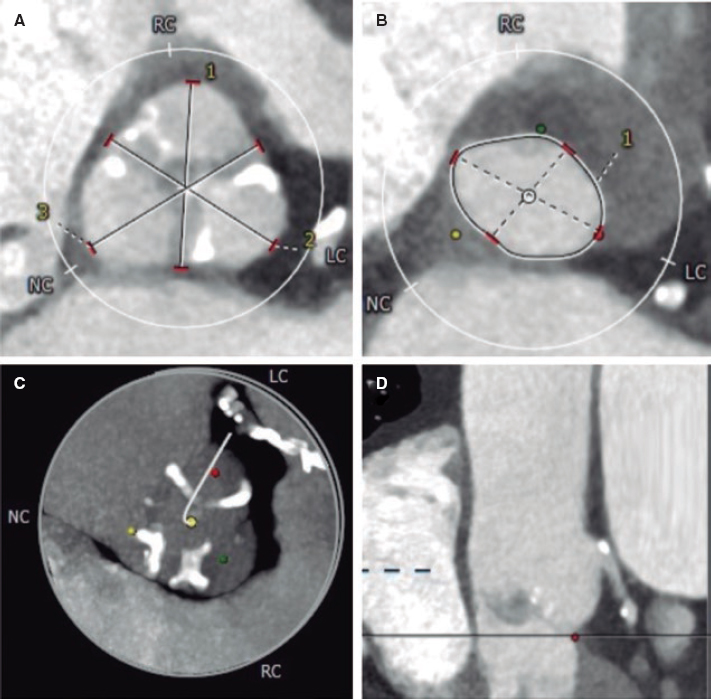
After diagnosis of a variant of the platypnea-orthodeoxia syndrome known as PFO related exercise-induced desaturation, the right heart catheterization confirmed the absence of pulmonary hypertension and then the percutaneous closure of the defect using an Occlutech ASD 13 device with a 28.5 mm left disc. The patient was discharged the next day.
Two weeks later, she joined the cardiac rehabilitation unit, where the new treadmill exercise stress testing conducted (figure 1B,D,F) confirmed the patient’s improved functional capacity and without desaturation.
PFO related exercise-induced desaturation is a rare and likely underdiagnosed condition that requires a high level of suspicion. Listening to and interacting with the patient is key to be able to diagnose this condition as it allows us to see, in situ, the drop of oxygen saturation that is indicative of a shunt. Without thorough history-taking and physical examination of the patient, we will be blind in our diagnostic process.
Exercise-induced desaturation should be considered in the presence of both exertional dyspnea and desaturation with exercise. However, to achieve diagnosis, a pulse oximeter should be put on the patient who should also be told to go for a walk. This is not a common practice though. Confirmation comes through an echocardiogram that shows the right-to-left shunt through the PFO.
Very few series have been published on this condition being the study conducted by Devendra et al.3 worth mentioning. They reported a series of 10 cases where closure of the PFO resolved the shunt and exercise-induced desaturation, which improved the patients’ functional capacity.
The mechanisms involved in right-to-left shunting in PFO related exercise-induce desaturation are still not fully understood. However, several may be involved to varying degrees of significance in each patient.5 During exercise, terrestrial gravity and muscular effort change the anatomical arrangement of the chest cavity, viscera, blood vessels, and filling pressures of the different cardiac chambers. In cases of diagnostic uncertainty, exercise right heart catheterization can be useful to screen for other causes of right ventricular failure like early pulmonary vasculopathy or changes to the diastolic dysfunction that can compromise cardiac output after closure.
Patients who develop PFO related exercise-induce desaturation may remain asymptomatic for years. However, as they age, pressure or anatomical changes (chest cavity changes, interatrial septum modification or aortic dilatation/elongation,6 among others) may redirect blood flow from the vena cava towards the PFO.4 This facilitates the passage of deoxygenated blood from the right atrium to the left cavities even in the absence of a significant pressure difference.5
The use of a device to close the atrial septal defect was decided because the PFO tunnel intermittently detached widely, leaving a wide trajectory. Similarly, the goal here was to make sure that the diameter of discs would adapt, as closely as possible, to the length of the septum, allowing them to embrace the septal aneurysm almost in its entirety and reduce device mobility after implantation.
This case is an example of the significant clinical impact that follows the occurrence of this condition and demonstrates that the percutaneous closure of the PFO is a safe and effective strategy.
The patient’s written informed consent and authorization was obtained to publish both figures and videos.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
V. Juárez, O. González, and C. Contreras drafted the manuscript preliminary version and selected the figures. A. Castro, A. Jurado, and S. Jiménez conducted the manuscript critical review by providing comments in later changes and reviewed its final version.
CONFLICTS OF INTEREST
None reported.
SUPPLEMENTARY DATA
Vídeo 1. Juárez Olmos VM. DOI: 10.24875/RECICE.M23000388
REFERENCES
1. Cruz-González I, Solis J, Inglessis-Azuaje I, Palacios IF. Patent foramen ovale: current state of the art. Rev Esp Cardiol. 2008;61:738-751.
2. Pristipino C, Germonpré P, Toni D, et al. European position paper on the management of patients with patent foramen ovale. Part II - Decompression sickness, migraine, arterial deoxygenation syndromes and select high-risk clinical conditions. Eur Heart J. 2021;42:1545-1553.
3. Devendra GP, Rane AA, Krasuski RA. Provoked exercise desaturation in patent foramen ovale and impact of percutaneous closure. JACC Cardiovasc Interv. 2012;5:416-419.
4. Punzengruber G, Kolb R, Meier B, Binder RK. Percutaneous closure of a patent foramen ovale causing exercise hypoxemia: Case report and a review of the literature. Catheter Cardiovasc Interv. 2021;98:733-737.
5. Agrawal A, Palkar A, Talwar A. The multiple dimensions of Platypnea-Orthodeoxia syndrome: A review. Respir Med. 2017;129:31-38.
6. Siniorakis E, Arvanitakis S, Skandalakis N, Barlagiannis D. Elderly patient with platypnea-orthodeoxia: check the ascending aorta. Rev Esp Cardiol. 2011;64:1074-1075.
* Corresponding author.
E-mail address: victormanuel.juarez@salud.madrid.org (V.M. Juárez Olmos).