A 52-year-old woman with atrial fibrillation, thrombocytopenia, and severe gastrointestinal bleeding while on several anticoagulants was referred for left atrial appendage closure. A year earlier, pulmonary vein ablation had been attempted but femoral access proved impossible due to a previously undetected congenital interruption of the inferior vena cava (figure 1A; asterisk). A right transjugular procedure was planned under general anesthesia and guided by transesophageal echocardiography and computed tomography-fluoroscopy fusion imaging (video 1 of the supplementary data). The left atrial appendage had a windsock morphology, with a mean diameter of 20 mm at the landing zone and 30 mm at the ostium (figure 1B,C). Consequently, a 24 mm x 30 mm LAmbre LAA Occluder system (LifeTech Scientific, China) was used, because its secure anchorage and closure mainly through the disk could facilitate the procedure. Transseptal puncture was performed using an SL1 sheath and a BRK-1 XS needle (Abbott, United States) by pre-shaping a secondary curve, followed by the insertion of a SafeSept guidewire (Pressure Products, United States) specifically designed for greater accuracy of transseptal puncture (figure 2A,B; the asterisk indicates the posterior and mid-puncture. Ao, aorta; LAA, left atrial appendage; SVC, superior vena cava). The device was implanted through a 10-Fr Fustar steerable sheath (LifeTech Scientific, China), which improved reach and coaxiality (figure 3A,B. E, extension; I, impulse; LOM, ligament of Marshall; MV, mitral valve; PR, posterior rotation). The patient was discharged at 24 hours without complications and on apixaban therapy (2.5 mg for 45 days).
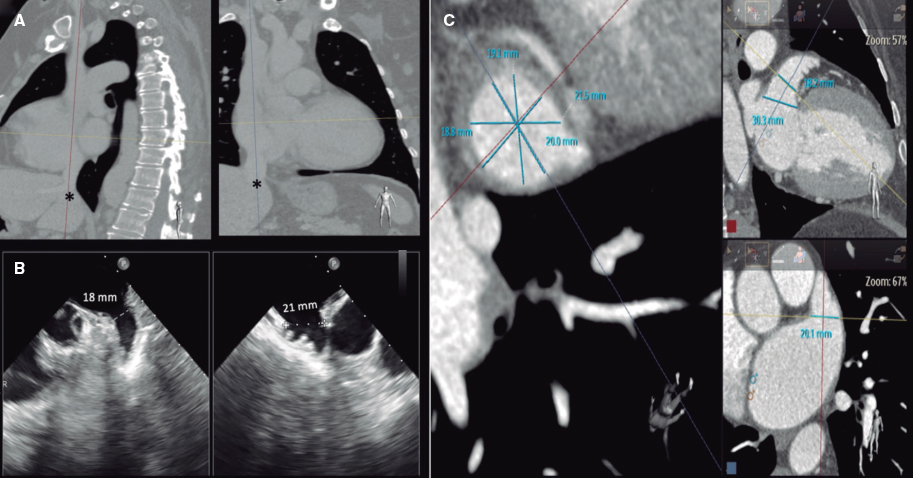
Figure 1.
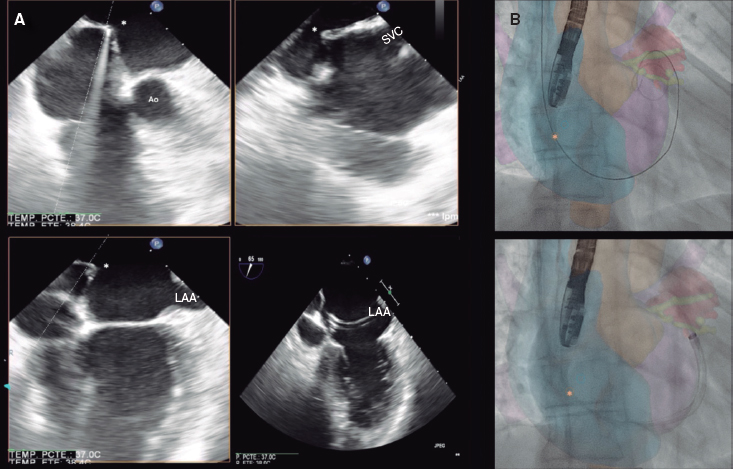
Figure 2.
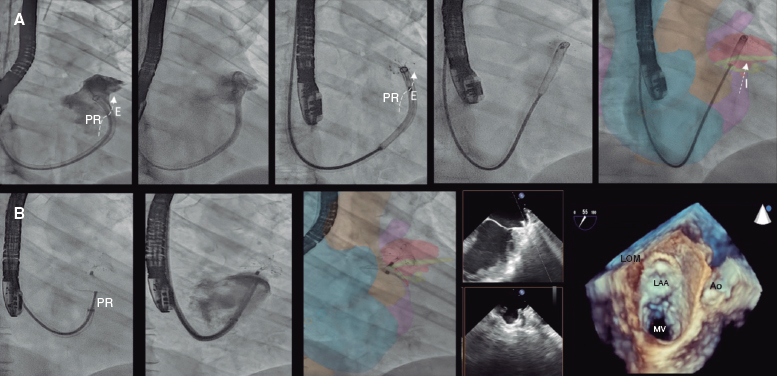
Figure 3.
Multimodal imaging, tools that facilitate precise transseptal puncture, and steerable sheaths can simplify the performance of procedures via upper access with efficiency and safety.
FUNDING
None declared.
ETHICAL CONSIDERATIONS
This work was published after approval was obtained from the research ethics committee of Complejo Hospitalario Universitario de Albacete, Spain. The patient gave her prior written informed consent to the intervention and publication of her case. Sex and gender variables were taken into consideration based on the SAGER guidelines.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
No artificial intelligence tool has been used during the preparation of this work.
AUTHORS’ CONTRIBUTIONS
All the authors participated in the drafting of this manuscript: J.G. Córdoba-Soriano was involved in drafting and design tasks, J.C. García-López in image selection and manuscript revision, and J. Jiménez-Mazuecos in manuscript revision and proofreading.
CONFLICTS OF INTEREST
None declared.
SUPPLEMENTARY DATA
Vídeo 1. Córdoba-Soriano JG. DOI: 10.24875/RECICE.M23000410











