Although the most common cause for coronary embolism is atrial fibrillation, we should take other conditions into consideration that, despite their low frequency of occurrence, need to be discarded to be able to establish a definitive treatment. Arteriovenous malformations like the case presented here are some of these conditions.
A 36-year-old woman with Rendu-Osler-Weber syndrome and recurrent and spontaneous epistaxis as the only personal medical history presented to the ER with oppression in her middle chest and pain radiating towards her left upper limb and back with concomitant vegetative symptoms. The electrocardiogram confirmed the presence of a subepicardial lesion in leads V2-V3 with high-sensitive troponin peak values of 9148 pg/mL.
A coronary angiography performed early confirmed the presence of a thrombus at the circumflex artery distal bifurcation (figure 1, arrow).
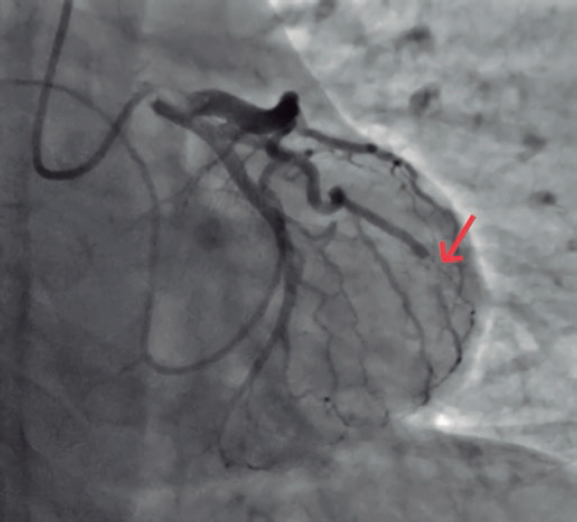
Figure 1.
To discard emboligenic source a Doppler ultrasound scan of the lower limbs was performed that revealed no signs of deep venous thrombosis. Given the patient’s syndromic history, a thoracic computed tomography angiography was performed to look for pulmonary arteriovenous fistulas and found 2 of them: one located at the left pulmonary territory in the posterior basal segment (figure 2, arrow) and another smaller one in the homolateral lateral basal segment.
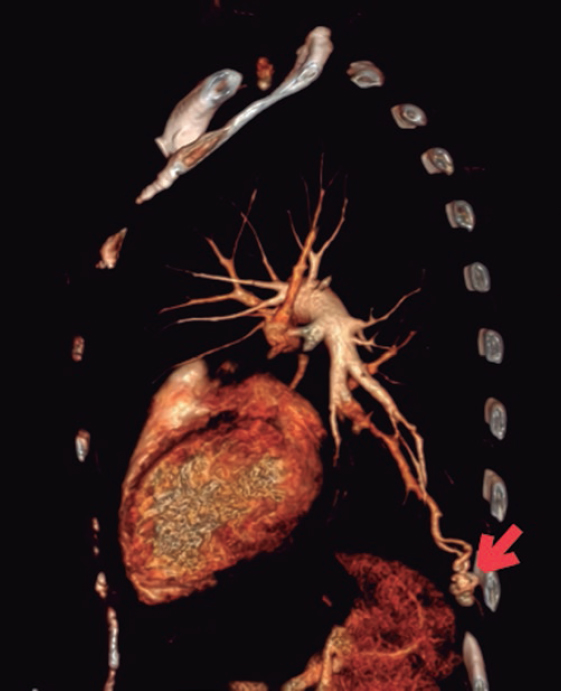
Figure 2.
The interventional cardiovascular unit used selective microcatheterization of the segmental arteries afferent to the fistulas and coil embolization to close them (figure 3, arrows).
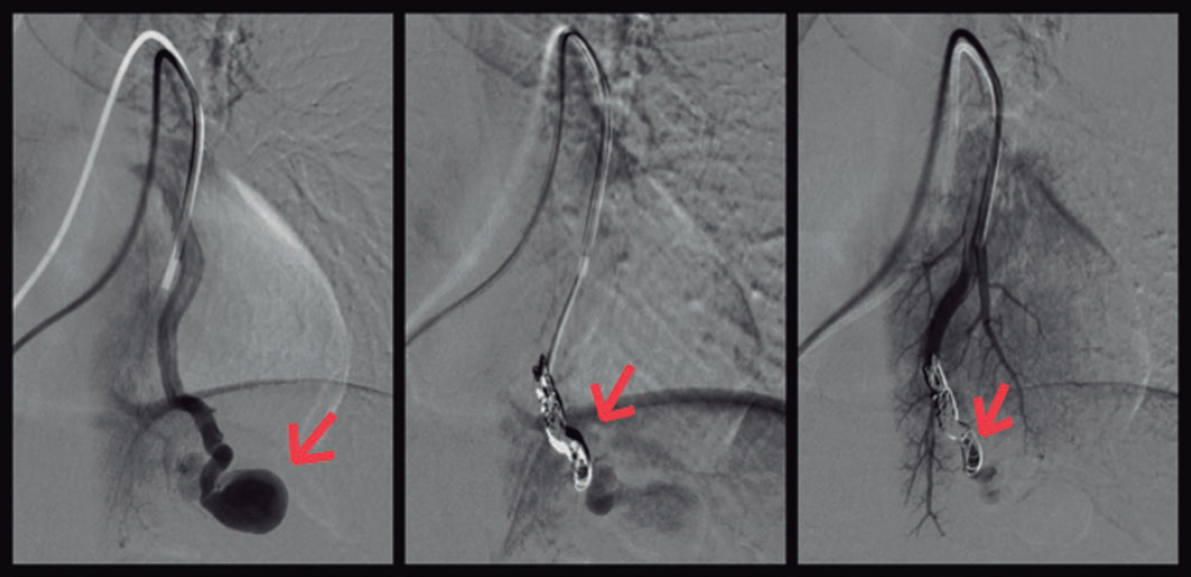
Figure 3.
Corresponding author: Unidad de Cuidados Intensivos Cardiológicos, Hospital Universitario Clínico San Cecilio, Avda. del Conocimiento s/n, 18016 Granada, Spain.
E-mail address: antoniocarranzapinel.ac@gmail.com (A. Carranza Pinel).











