Finalist case in the ACCIS 2023 Madrid course
We report the case of a 53-year-old male patient who required venoarterial extracorporeal membrane oxygenation (VA-ECMO) after a refractory cardiac arrest due to a ventricular fibrillation secondary to an anterolateral myocardial infarction. The cannulation was performed with a 25-Fr × 55 cm drain (right femoral vein) and a 17-Fr × 15 cm return (left common femoral artery). An intra-aortic balloon pump (IABP) was inserted through the right femoral artery (7-Fr). After stabilization, both the VA-ECMO and IABP were retrieved. The arterial insertion points were sealed with a Perclose ProGlide (Abbott, United States) system and the venous site with manual compression.
Shortly afterward, the patient developed shock accompanied by hypoperfusion in the right leg (indicated by near-infrared spectroscopy readings of 17% in the right leg vs 59% in the left leg). No changes were evident on electrocardiography, echocardiography, or coronary angiography. The arterial pressure waveform analysis revealed high cardiac output, increased central venous pressure, and a low systemic vascular resistance index. Computed tomography angiography revealed a high-flow arteriovenous fistula between the right femoral vein and artery (figure 1; red arrow shows a tubular communication between the 2 vessels). To assess the hemodynamic impact of the fistula, a 10-minute compression test was conducted (table 1 and figure 2), demonstrating an increase in mean arterial pressure, a decrease in cardiac output and left ventricular outflow tract velocity-time integral, and a significant reduction in central venous oxygen saturation.
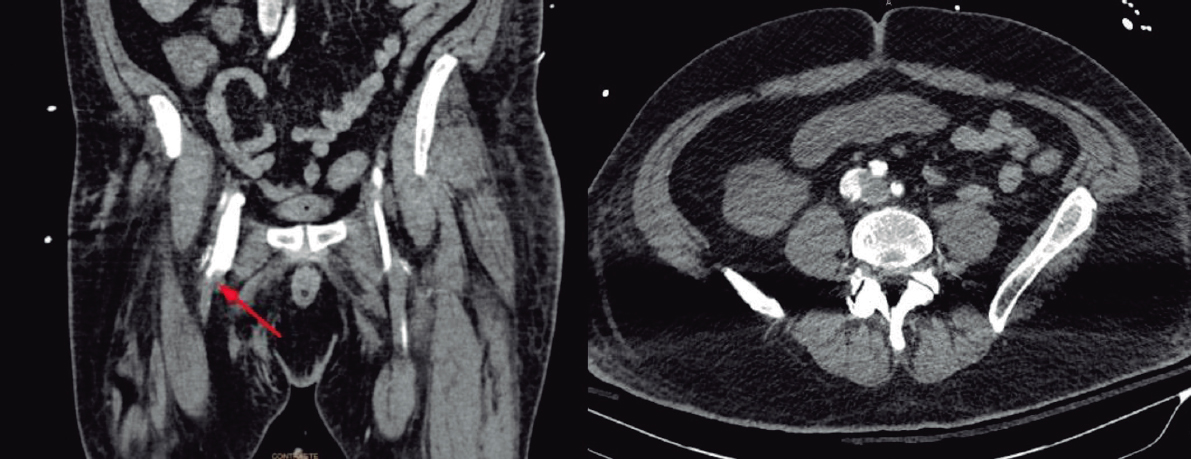
Figure 1.
Table 1. Changes pre- and post-compression of AVF
| Pre-procedure | Post-procedure | |
|---|---|---|
| Hemodynamic | ||
| mPA (mmHg) | 48 | 62 |
| Heart rate (bpm) | 98 | 95 |
| Systolic volume (mL) | 46 | 38 |
| CO (L/min) | 4,5 | 3,6 |
| CI (L/min/m2) | 2,2 | 1,8 |
| IVC (mmHg) | 25 | 22 |
| Echocardiogram | ||
| LVOT-VTI (cm2) | 13,4 | 9,2 |
| RVEDV (mm) | 45 | 38 |
| TAPSE (mm) | 13 | 22 |
| Gasometry | ||
| SvO2 (%) | 87,9 | 60,7 |
| PpaO2 (mmHg) | 97 | 104 |
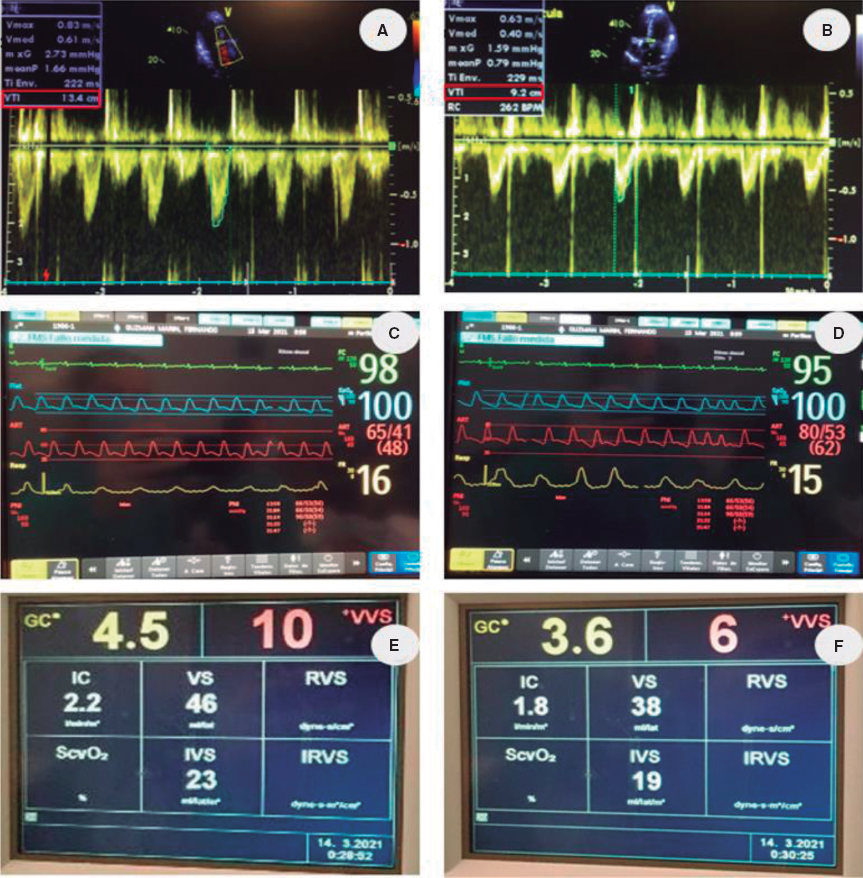
Figure 2.
After demonstrating the hemodynamic impact of the fistula, vascular surgeons treated it by surgically implanting an intravascular stent (Viabahn 8 × 100 mm, GORE, United States) in the right superficial femoral artery. The intervention resulted in significant hemodynamic and respiratory improvement and recovery of perfusion in the right leg.
FUNDING
The authors did not receive support from any organization for the submitted work.
ETHICAL CONSIDERATIONS
This work was conducted following the ethics recommendations of our hospital, although no ethics review approval was required in human participants in accordance with the local legislation and institutional requirements. Oral consent was obtained from the patient and his family. The anonymity of the patient was respected at all times. In our research, we always try to adhere to the SAGER guidelines.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
No artificial intelligence tool was used to prepare this paper.
AUTHORS’ CONTRIBUTIONS
P. Torrella and M. Vidal provided care for the study patient and conceived the study and its design. All authors critically reviewed and approved the study.
CONFLICTS OF INTEREST
The authors have no conflict of interest to declare.











