ABSTRACT
Introduction and objectives: Patients with left main coronary artery (LMCA) stenosis have been excluded from the trials that support the non-inferiority of the instantaneous wave-free ratio (iFR) compared to the fractional flow reserve (FFR) in the decision-making process of coronary revascularization. This study proposes to prospectively assess the concordance between the two indices in LMCA lesions and to validate the iFR cut-off value of 0.89 for clinical use.
Methods: National, prospective, and observational multicenter registry of 300 consecutive patients with intermediate lesions in the LMCA (angiographic stenosis, 25% to 60%. A pressure gudiewire study and determination of the RFF and the iFR will be performed: in the event of a negative concordant result (FFR > 0.80/iFR > 0.89), no treatment will be performed; in case of a positive concordant result (FFR ≤ 0.80/iFR ≤ 0.89), revascularization will be performed; In the event of a discordant result (FFR> 0.80/iFR ≤ 0.89 or FFR ≤ 0.80/iFR> 0.89), an intravascular echocardiography will be performed and revascularization will be delayed if the minimum lumen area is > 6 mm2. The primary clinical endpoint will be a composite of cardiovascular death, LMCA lesion-related non-fatal infarction or need for revascularization of the LMCA lesion at 12 months.
Conclusions: Confirm that an iFR-guided decision-making process in patients with intermediate LMCA stenosis is clinically safe and would have a significant clinical impact. Also, justify its systematic use when prescribing treatment in these potentially high-risk patients.
Registered at ClinicalTrials.gov ( Identifier: NCT03767621).
Keywords: iFR. FFR. Left main coronary artery.
RESUMEN
Introducción y objetivos: Los pacientes con estenosis en el tronco coronario izquierdo (TCI) han sido excluidos de los ensayos que apoyan la no inferioridad del cociente de presiones en el índice diastólico instantáneo sin ondas (iFR) respecto a la reserva fraccional de flujo (RFF) en la toma de decisiones sobre revascularización coronaria. El presente estudio propone valorar de manera prospectiva la concordancia entre los dos índices en lesiones del TCI y validar el valor de corte del iFR de 0,89 para su uso clínico.
Métodos: Registro multicéntrico nacional, prospectivo, observacional, con la inclusión de 300 pacientes consecutivos con lesiones intermedias (estenosis angiográfica 25-60%) en el TCI. Se realizará un estudio con guía de presión y determinación de RFF e iFR. En caso de resultado concordante negativo (RFF > 0,80 / iFR > 0,89), no se realizará tratamiento; en caso de resultado concordante positivo (RFF ≤ 0,80 / iFR ≤ 0,89), se realizará revascularización; en caso de resultado discordante (RFF > 0,80 / iFR ≤ 0,89 o RFF ≤ 0,80 / iFR > 0,89), se realizará estudio con ecocardiografía intravascular y se considerará diferir la revascularización si el área luminal mínima es > 6 mm2. El criterio de valoración clínico primario será la incidencia del combinado de muerte cardiovascular, infarto no mortal relacionado con la lesión del TCI o necesidad de revascularización de la lesión del TCI a los 12 meses.
Conclusiones: La demostración de la seguridad clínica en la toma de decisiones del iFR en pacientes con lesiones intermedias en el TCI tendría un impacto clínico importante y justificaría su uso sistemático para la decisión del tratamiento en estos pacientes de potencial alto riesgo.
Registrado en ClinicalTrials.gov (identificador: NCT03767621).
Palabras clave: iFR. RFF. Tronco coronario izquierdo.
Abbreviations MLA: minimum lumen area. FFR: fractional flow reserve. iFR: instantaneous wave-free ratio. IVUS: intravascular ultrasound. LMCA: left main coronary artery.
INTRODUCTION
Assessing functional severity of coronary stenoses at left main coronary artery (LMCA) level through coronary angiography has serious limitations.1 To treat angiographically intermediate stenoses (25% to 60% diameter) the use of invasive (ultrasound or optical coherence tomography) or functional imaging modalities (determining fractional flow reserve [FFR] to indicate the need for revascularization) has been proposed.2 Patients with LMCA stenosis have traditionally been excluded from randomized clinical trials that assessed the prognostic capabilities of the functional assessment of coronary stenoses through the use of FFR.3-5 The use of FFR to assess LMCA stenoses is backed by a limited number of non-randomized clinical trials that confirmed that FFR values > 0.80 is associated with a low risk of events if no revascularization is performed in patients with intermediate LMCA stenoses.6
The instantaneous wave-free ratio (iFR) is a new, easier-to-use, and cost-effective invasive index to assess the coronary function compared to FFR since there is no need to induce maximum coronary hyperemia to estimate it.7 Although a non-inferior prognostic value of iFR compared to the FFR has recently been confirmed in patients with intermediate lesions in 2 large trials, the presence of LMCA lesions was largely anecdotal or inexistent in both indices.8,9 However, a non-randomized clinical trial has been published with a similar design to those previously conducted with the FFR that provides encouraging data on the value of iFR in the decision-making process regarding the LMCA. However, in such trial, the FFR—the most widely used index to assess intermediate LMCA stenoses—was not determined at the same time, which means that the results of this registry cannot be put into context.10 Also, there are signs that the location of the LMCA lesion is a predictor of worse concordance between both indices.11
Proving the clinical safety of iFR in patients with intermediate LMCA lesions would have a major clinical impact and justify its systematic use in the decision-making process regarding the management of these high-risk patients.
The objective of this study is to assess the concordance between 2 physiological indices—the FFR and the iFR—in the assessment of intermediate LMCA lesions. Also, to validate prospectively the clinical safety profile of a revascularization strategy based on an iFR cut-off value of 0.89.
METHODS
Study design
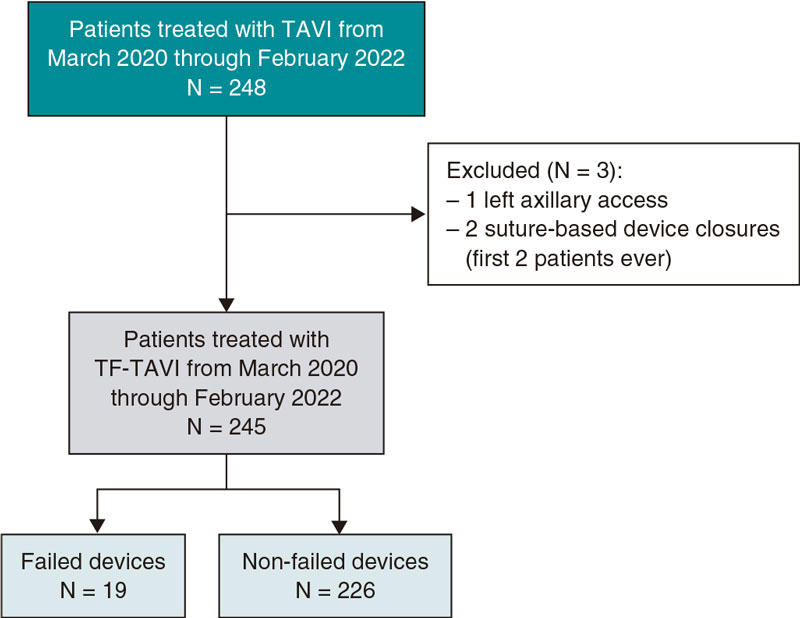
National, prospective, observational, and multicenter registry including 300 consecutive patients with intermediate LMCA lesions (25% to 60% angiographic stenosis). A study will be conducted in all patients using intracoronary guidewire pressures. Also, both the FFR and the iFR values will be determined distal to the LMCA. Per protocol it is advised that the indication for revascularization should be decided based on the result of the iFR in such a way that:
– In patients with iFR and FFR values in the LMCA lesion > 0.89 and > 0.80, respectively clinical follow-up without LMCA lesion revascularization is indicated. In the presence of other lesions outside the LMCA with percutaneous revascularization criteria, the revascularization of these other lesions is indicated.
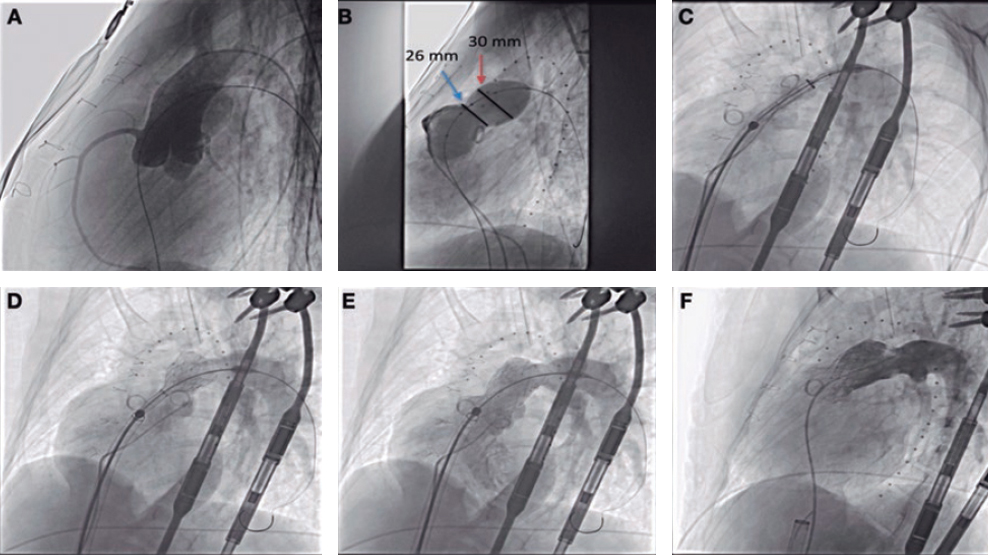
– In patients with iFR and FFR values in the LMCA lesion ≤ 0.89 and ≤ 0.80, respectively the revascularization of the LMCA lesion is indicated (percutaneous through a drug-eluting stent or surgical). In the presence of other lesions outside the LMCA with revascularization criteria (whether percutaneous or surgical), the revascularization of these other lesions is indicated.
– In case of discrepancy between the FFR and the iFR (positive vs negative or vice versa with 2 or more points above or below the respective cut-off value) an intravascular ultrasound (IVUS) should be performed to decide whether to indicate revascularization or not; with minimum lumen areas (MLA) > 6 mm2 revascularization is ill-advised.
Patients whose management is not consistent with what the iFR value recommends will not be addressed for the strategy safety analysis, and clinical outcomes will be assessed separately.
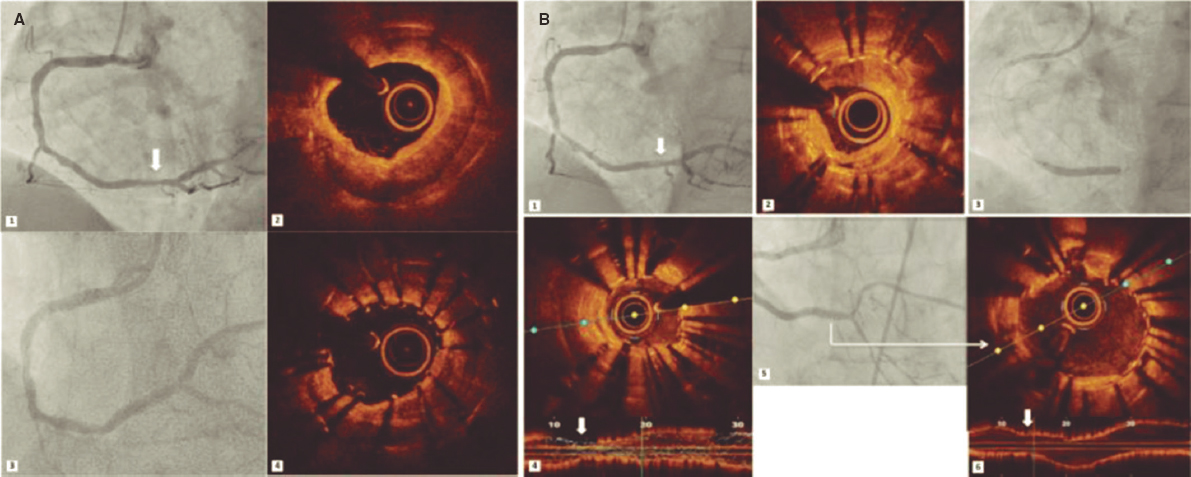
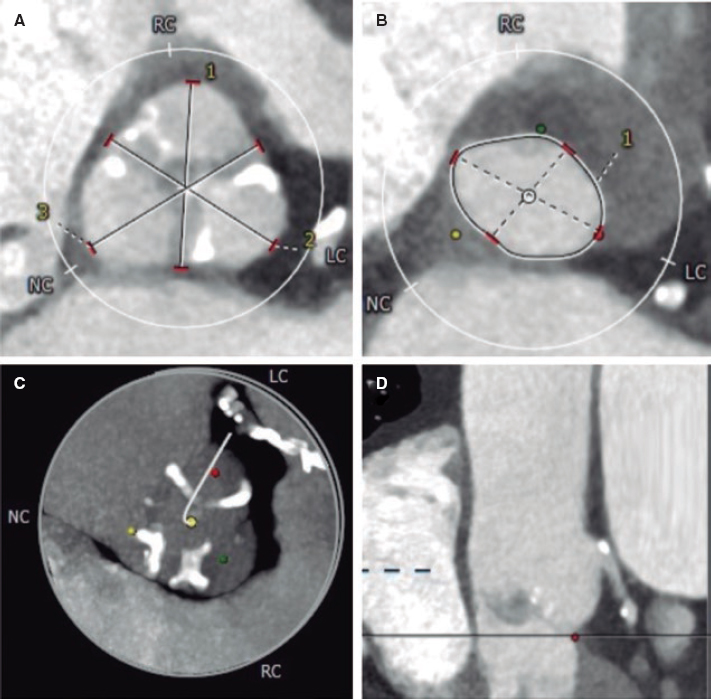
Figure 1 shows the decision-making algorithm based on FFR and iFR results. IVUS is indicated in controversial cases, and recommended in the remaining cases to determine the correlation between the MLA and the iFR.
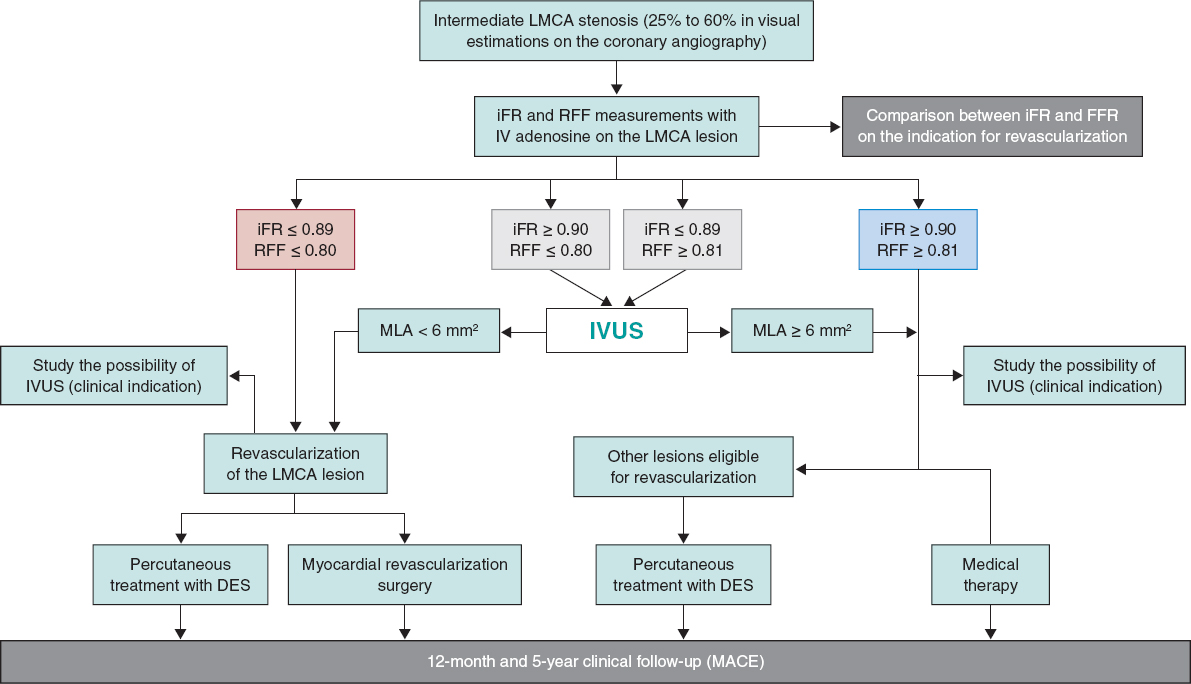
Figure 1. Decision-making algorithm based on the FFR and iFR results. DES, drug-eluting stent; FFR, fractional flow reserve; iFR, instantaneous wave-free ratio; IV, intravenous; IVUS, intravascular ultrasound; LMCA, left main coronary artery; MACE, major adverse cardiovascular events, MLA, minimum lumen area.
In patients eligible for percutaneous treatment, IVUS is highly recommended, and its utility will be assessed prospectively during the planning and optimization of the procedure.
Clinical follow-up is advised from 12 months to 5 years to determine the prognostic primary endpoint by assessing a composite endpoint of cardiovascular death, LMCA lesion-related non-fatal infarction or need for LMCA revascularization at the 12-months and 5-year follow-up.
Notifications
The study has been approved by the reference ethics committee and notified to the local ethics committee of all participant centers. The study has been registered in Clinicaltrials.gov with registration number NCT03767621. Devices with CE marking have only been used, and only for the indications already approved. The study observes the principles established by the Declaration of Helsinki. All patients gave their prior written informed consent to participate in the study.
Study population
Patients with suspected or confirmed ischemic heart disease on whom a coronary angiography is performed that detects intermediate angiographic LMCA stenoses (between 25% and 60%). Also, patients in whom intracoronary pressure guidewires are used to determine the iFR and the FFR in the LMCA lesion to decide on the indication for myocardial revascularization—whether percutaneous with a DES or surgical—based on the indication considered more appropriate.
Inclusion and exclusion criteria are shown on table 1. In cases of severe lesions at left anterior descending coronary artery or left circumflex artery level, the patient will not be included in the study unless the LMCA lesion is assessed after the percutaneous treatment of these lesions while taking into account that, if the LMCA lesion is significant, treatment will be percutaneous.
Table 1. Inclusion and exclusion criteria of the iLITRO-EPIC-07 trial
| Inclusion criteria |
| Patients with intermediate LMCA lesions (25% to 60% angiographic stenosis on visual estimations) eligible for a pressure guidewire study to determine the iFR |
| Patients aged ≥ 18 years |
| Patients capable of giving their informed consent |
| Exclusion criteria |
| Patients with an indication for coronary artery bypass graft regardless of the significance of the LMCA lesion |
| Patients with LMCA lesions showing ulceration, dissection or thrombus |
| Patients with lesions in a previously non-dysfunctional arterial or venous graft in the territory irrigated by the LMCA (protected LMCA) |
| Patients with acute coronary syndrome with potentially culprit lesion in the LMCA |
| Patients incapable of giving their informed consent |
iFR, instantaneous wave-free ratio; LMCA, left main coronary artery. |
Study endpoints
The iLITRO-EPIC 07 trial has 2 primary endpoints:
1) To establish concordance before indicating revascularization between 2 invasive functional assessment indices through intracoronary pressure guidewire in intermediate LMCA lesions with FFR and iFR cut-off values ≥ 0.80 (with IV adenosine) and ≥ 0.89 to delay treatment.
2) To validate prospectively the safety profile associated with the decision-making process regarding the revascularization of intermediate LMCA stenoses based on an iFR cut-off value of 0.89 measured using an intracoronary pressure guidewire to decide whether to revascularize or not based on the number of patients with delayed LMCA revascularization of the composite endpoint of cardiovascular death, LMCA lesion-related non-fatal infarction or need for LMCA revascularization at the 12-month follow-up.
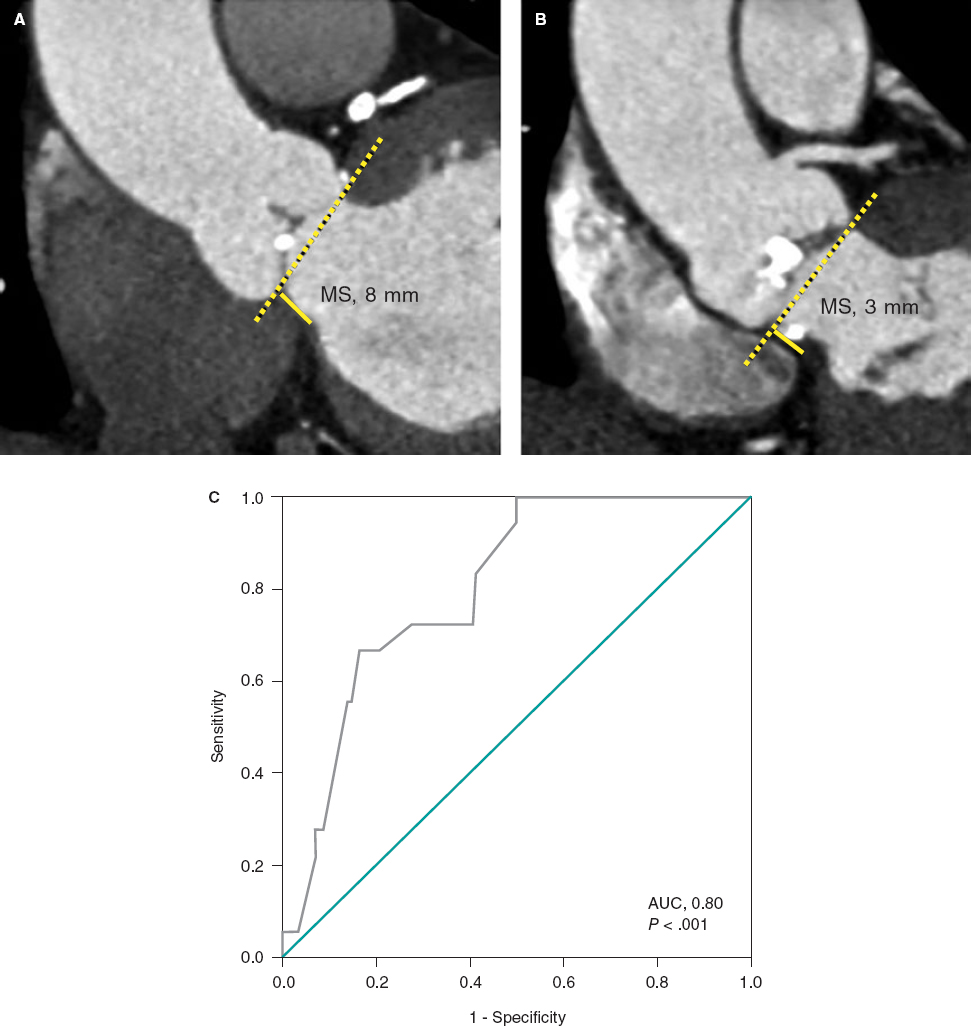
Secondary endpoints are to determine the correlation between the iFR value in these lesions and the MLA determined by the IVUS and the utility of IVUS for the planning and optimization of LMCA lesions (table 2).
Table 2. Secondary endpoints of the iLITRO-EPIC-07 trial
| Correlation between the assessment obtained through pressure guidewire (iFR) and the minimum lumen area measured through IVUS |
| Role of IVUS in the planning of treatment in the subgroup of patients treated with percutaneous therapy |
| Role of IVUS in the optimization of treatment in the subgroup of patients treated with percutaneous therapy |
| All-cause mortality at 12 months and 5 years |
| Cardiovascular death at 12 months and 5 years |
| Non-fatal infarction at 12 months and 5 years |
| LMCA lesion-related non-fatal infarction at 12 months and 5 years |
| Revascularization at 12 months and 5 years |
| Myocardial infarction associated with the revascularization of the LMCA (whether percutaneous or surgical) |
| Thrombosis of 1 or several stents in the LMCA at 12 months and 5 years |
| Restenosis of 1 or several stents in the LMCA at 12 months and 5 years |
| New target lesion revascularization in the LMCA (whether percutaneous or surgical) at 12 months and 5 years |
iFR, instantaneous wave-free ratio; LMCA, left main coronary artery; IVUS: intravascular ultrasound. |
Study procedure
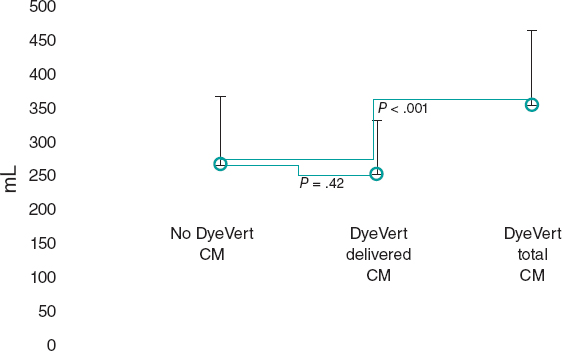
Figure 2 shows the procedure methodology on a flowchart.
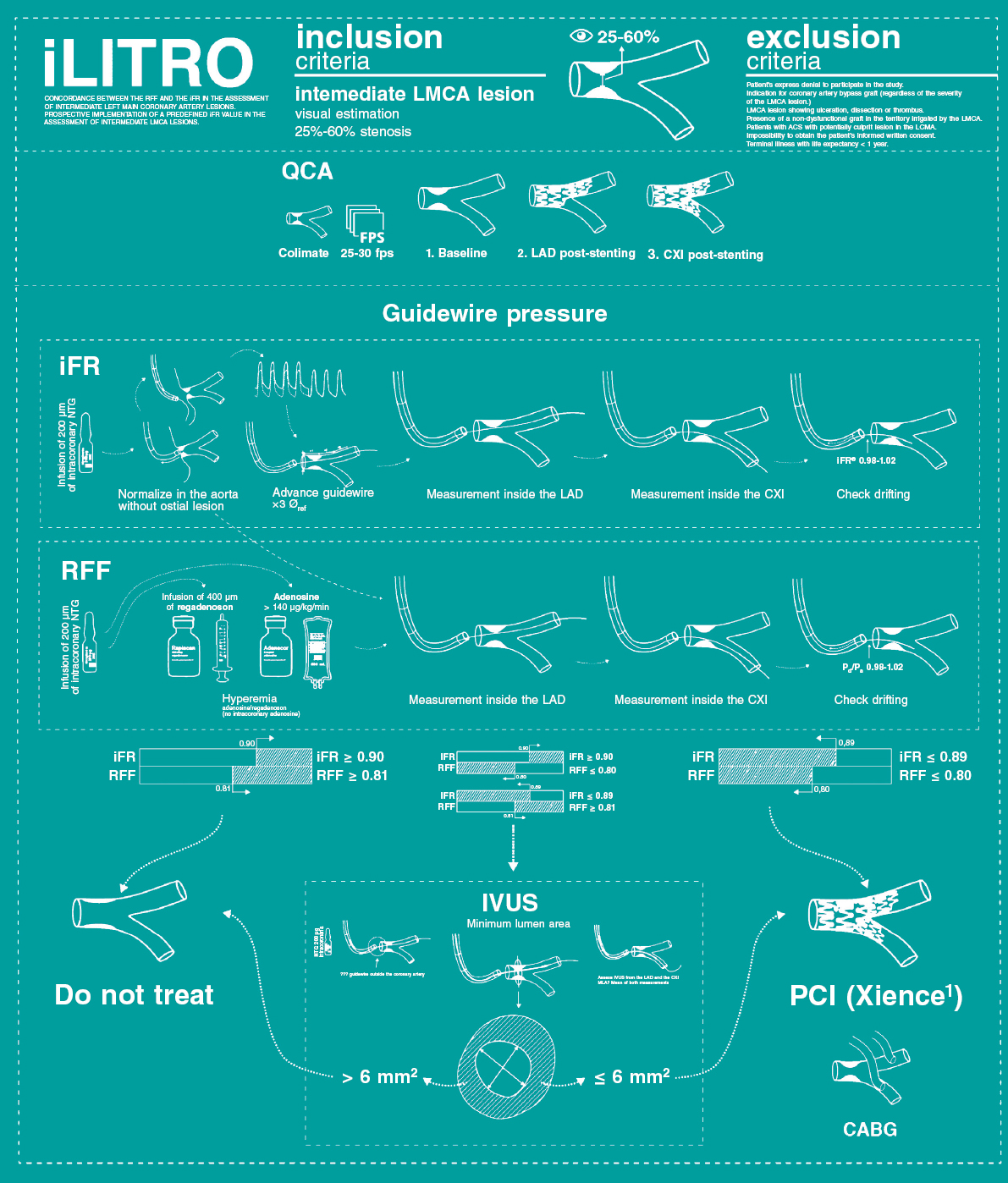
Figure 2. Study protocol and procedures. ACS, acute coronary syndrome; CABG, coronary artery bypass graft; FFR, fractional flow reserve; iFR, instantaneous wave-free ratio; IVUS, intravascular ultrasound; LAD, left anterior descending coronary artery; LCX, left circumflex artery; LMCA, left main coronary artery; MLA, minimum lumen area; PCI, percutaneous coronary intervention; QCA, quantitative coronary angiography.
Protocol to perform a study using a pressure guidewire
The patient is eligible for functional assessment in the presence of intermediate LMCA stenoses with visual estimations on the coronary angiography between 25% and 60%.
After catheterization using a guide catheter, at least, 200 µg of intracoronary nitroglycerin should be administered to keep coronary reactivity under control. Afterwards, the intracoronary guidewire should be advanced with the sensor placed in the ostium of the guide catheter; also, pressure curves should be brought back to normal for 5 to 10 heart beats. if the lesion has an ostial location, normalization will occur by removing the guide catheter from the coronary artery and placing the guidewire into the aorta. Afterwards, the guidewire should be removed from the catheter, and coronary catheterization performed to advance the guidewire.
The pressure guidewire should be advanced until, at least, 3 times the diameter of the vessel beyond the most distal stenosis to be able to measure the iFR according to the standard protocol.
After measuring the iFR, the guidewire should be removed with pressure curve monitorization until the inside of the guide catheter. At this point, the presence of the pressure calibration loss phenomenon (drifting) should be discarded. In case of overt drift (Pd/Pa measured on the catheter tip < 0.98 or > 1.02) measures should be taken again.
Afterwards, the FFR will be determined during hyperemia through the administration of adenosine in continuous IV infusion at doses ≥ 140 µg/kg/min for, at least, 2 minutes or an IV bolus of 0.4 mg of regadenoson.
After measuring the FFR, the guidewire should be removed with pressure curve monitorization until the inside of the guide catheter. At this point, the presence of drifting should be discarded. In case of overt drift (Pd/Pa measured on the catheter tip < 0.98 or > 1.02) measures should be taken again.
In case of discrepancy between the results of the FFR and the iFR (FFR ≤ 0.80 with iFR ≥ 0.90 or FFR ≥ 0.81 with iFR ≤ 0.89) IVUS will be performed, and the MLA determined. Revascularization will be indicated with MLAs < 6 mm2 based on the results from the LITRO trial.12
Protocol to conduct IVUS studies
IVUS studies will be mandatory if the FFR and the iFR disagree. In patients eligible for percutaneous treatment of their LMCA lesions, the IVUS is highly recommended to guide the procedure. In the remaining patients (when iFR-guided medical therapy or surgical revascularization is decided) the IVUS is recommended to establish the correlation between the iFR value and the MLA measured on the LMCA whenever possible. The IVUS system used can be mechanical or rotational with resolutions between 20 MHz and 60 MHz.
An 0.014 in intracoronary guidewire will be advanced to perform the IVUS study (it can be the same pressure guidewire used to determine the iFR) towards the left anterior descending or left circumflex coronary arteries. After the administration of 200 µg of intracoronary nitroglycerin, the IVUS catheter will be advanced distal to the LMCA bifurcation. Afterwards, the catheter will be manual or automatically removed until the ascending aorta. It is essential that the guide catheter should remain outside the coronary artery to study the left main coronary artery entirely including its ostial region. The catheter will be placed in the left anterior descending coronary artery (preferably) or left circumflex artery or both (to conduct 2 studies with MLA determination from these positions and eventually pick the one with the lowest values).
In cases of catheter backward jump, even on manual mode (with calcified angulation) it is recommended to move the catheter forward from the aorta to acquire images of the region of interest that had not been properly assessed.
Technical aspects of the assessment of left main coronary artery lesions through fractional flow reserve
The study of LMCA lesions using pressure guidewires has some particularities that should be addressed when conducting the study.
Location of the lesion
A total of 3 different possible lesion locations can be anatomically distinguished on the LMCA depending on whether there is damage to the ostium, body or distal portion (bifurcation). The location of the lesion inside the LMCA has implications when conducting the study with the pressure guidewire. When the lesion is found in the ostium or the body, catheterization should be coaxial. Non-coaxial catheterization involves contact of the catheter lumen with the vessel wall to the extent that it can dampen the aortic pressure and artificially elevate the value of the FFR. For this reason, non-selective catheterization is advised when equalizing or normalizing the catheter and guidewire pressures when the latter is placed distal to the lesion to measure the FFR during maximum hyperemia. When the lesion is found in the LMCA distal portion and there is damage to its origin and main branches, both the distal LMCA and each one of its branches should be treated as 1 functional unit regardless of the degree of damage to these branches. To estimate the FFR, measurements are taken from the left anterior descending and left circumflex coronary arteries. The LMCA lesion is considered functionally significantly when the measurements of either one of the 2 main vessels is < 0.80.
Induction of hyperemia
In the assessment of LMCA lesions the use of an intracoronary bolus of adenosine is ill-advised because, since the non-selective catheterization of the left coronary artery is required, part of the drugs administered never reach this coronary artery, which is why the induction of hyperemia can be suboptimal. For this reason, the IV administration of drugs whether adenosine (infusions of 140 µg/kg/min for, at least, 2 minutes) or regadenoson (doses of 0.4 mg in IV bolus) is advised.13
Presence of left anterior descending or left circumflex coronary artery lesions
The presence of 1 isolated LMCA lesion is not rare. A series of all-comers treated with diagnostic coronary angiography proved that, in patients with damage to the LMCA, only 9% had 1 single LMCA lesion, 17% had 1 LMCA lesion plus damage to 1 vessel, 35% had 1 LMCA lesion plus damage to 2 vessels, and 38% had LMCA disease plus damage to 3 vessels.14
Statistical analysis
Demographic, clinical, hemodynamic, and procedural data will be presented for the entire group. Continuous variables will be expressed as mean, and standard deviation (or if the distribution of the values do not follow a normal, as median, and interquartile range). Categorical variables will be expressed as frequencies and percentages. The data obtained will be studied using the unilateral analysis of variance (ANOVA) for the continuous variables, and Fisher’s exact test or the chi-square test for the categorical variables, when appropriate. When appropriate, non-parametric tests will be used with variables without a normal distribution or when normalization is not possible. The Kaplan-Meier survival curves will be presented for the previously specified criteria. The concordance analyses will be conducted using Cohen’s kappa coefficient. Also, sensitivity, specificity, positive and negative predictive values, and the area under the receiver operating characteristic (ROC) curve will be estimated.
Data curation and monitorization
Clinical, angiographic, physiological, and IVUS data will all be saved in a safe electronic CRD managed by Fundación EPIC, the promotor of the study. Clinical data at both the 12-month and 5-year follow-up, as well as the presence of cardiovascular events at the follow-up will also be saved in the same electronic CRD.
DISCUSSION
The iLITRO-EPIC 07 trial has a double primary endpoint: on the one hand, to establish the concordance between 2 intracoronary physiological indices, the FFR and the iFR, when assessing the severity of intermediate LMCA lesions; on the other hand, to study the use of a predetermined iFR value to indicate the revascularization of intermediate LMCA lesions with an up to 5-year clinical follow-up.
Left main coronary artery disease. Implications for the interventional cardiologist
Significant LMCA disease, understood as a stenosis in its greater diameter > 50%, is associated with a poor mid-term prognosis. Studies prior to coronary revascularization confirmed survival rates < 40% at the 4-year follow-up after diagnosis.15
The limitations of the angiographic assessment of the severity of LMCA lesions are well established.16-18 Before suggesting revascularization in a patient with LMCA lesions, in particular ostial lesions, it is important to know whether the lesion really needs to be revascularized, that is, whether it is hemodynamically significant. LMCA stenoses are found in between 4% to 9% of all diagnostic coronary angiographies.1 Due to their anatomical location, catheter-induced artifacts or to the severity of distal lesions, among other factors, interpreting LMCA lesions is associated with the highest intra- and inter-observer variability compared to lesions found in other parts of the coronary tree.16 When stenoses ≥ 50% were found in the CASS registry,19 a second observer confirmed that the stenosis was not significant in 19% of the cases.
Several former studies have confirmed that the prognosis of patients with functionally insignificant LMCA lesions is favorable.6 Also, that the surgical revascularization of hemodynamically insignificant lesions is associated with a high rate of early graft failure.20
The LITRO trial, led by the Spanish Society of Cardiology Working Group on Intracoronary Diagnostic Techniques, was a multicenter and prospective study. It proved that, in patients with angiographically intermediate LMCA lesions, the presence of a MLA ≥ 6 mm2 measured on the IVUS allows us to delay revascularization in a safely manner.12
Evidence to guide the revascularization of the left main coronary artery through functional assessment
To this date, no definitive data on the prognostic value of iFR measurements in intermediate LMCA stenoses have been published. The presence of a significant stenosis (> 70%) on the coronary angiography was an exclusion criteria in the DEFER, FAME, and FAME II clinical trials, as well as in the DEFINE FLAIR trial. Only the IFR SWEDEHEART trial included 30 patients with significant LMCA stenoses (1.6% of all the patients included).3-5,8,9 An observational and retrospective study of 314 patients confirmed that delaying the revascularization of the LMCA using a iFR cut-off value of 0.89 as the guide was safe at the 30-month clinical follow-up.10 However, in this observational registry the FFR, a widely validated index in the LMCA, was not obtained at the same time. This means that the results reported by this registry cannot be put into context and the concordance between both indices cannot be analyzed either.
The data available that support the use of the FFR in LMCA lesions come from several studies shown on table 1. The cut-off values used in these studies go from 0.75 to 0.80. In the study that has included, to this date, the highest number of patients with intermediate angiographic lesions, 213, only patients with FFR values < 0.80 were treated. However, in patients with higher values a conservative manage was used. No differences in the mortality or severe cardiovascular event rates were reported at the 5-year follow-up.6 Therefore, the reference FFR value for LMCA lesions, as well as the remaining lesions, is < 0.80.
A metanalysis that included data from 8 landmark studies found no differences in the primary endpoint of death, non-fatal myocardial infarction or revascularization. However, the need for revascularization was greater in the group on medical therapy: whether this was primarily due to the revascularization of the LMCA is still under discussion.21
A recent study that assessed the correlation between the FFR and the iFR values based on the location of the lesion studied revealed that such correlation was weaker when the lesion was found on the LMCA or in the proximal left anterior descending coronary artery compared to other locations. This was attributed to a greater amount of vessel-dependent myocardium in these proximal lesions. Taking the FFR value and an iFR cut-off value ≥ 0.89 as a reference, both the false positives (21.9%) and the false negatives (26.7%) were more evident when the lesion was found on the LMCA or the proximal left anterior descending coronary atery.11 Some studies have suggested that resting indices like the iFR could provide better measurements of coronary flow during hyperemia compared to the FFR.22,23 This means that using the FFR as the gold standard could be questionable in this setting. Also, the scientific evidence available indicates that the discrepancies seen between the iFR and the FFR are not associated with a worse prognosis.24 This means that the present study could clarify whether the iFR is associated with a weaker indication for revascularization in intermediate LMCA lesions with the exact same clinical safety compared to the FFR.
CONCLUSIONS
The iLITRO-EPIC 07 trial is the first prospective study to assess the concordance between the FFR and the iFR in intermediate LMCA lesions. Also, that it is safe to guide the indication for revascularization based on an iFR cut-off value of 0.89.
FUNDING
The promoter of the study, Fundación EPIC, has received an institutional research grant from Phillips Volcano (The Netherlands) to pay for the design and maintenance costs of the electronic CRD. Philips Volcano has not been involved in the design of the study or protocol whatsoever. Philips Volcano has not been involved in the development of the study whatsoever including recruitment, follow-up, data curation, result analysis and interpretation, writing or final approval of both the protocol and this manuscript. The authors are solely responsible for the study design, writing, edition, and final version of the manuscript.
AUTHORS’ CONTRIBUTIONS
All the authors are lead investigators of the iLITRO-EPIC07 trial at their corresponding working centers, collaborated in the writing of the study protocol, and in the recruitment of the patients. The manuscript was written by O. Rodríguez-Leor, J.M. de la Torre-Hernández, and A. Pérez de Prado; the remaining authors reviewed the manuscript.
CONFLICTs OF INTEREST
A. Pérez de Prado declared to have received fees from iVascular, Boston Scientific, Terumo, B. Braun, and Abbott Vascular. José M. de la Torre Hernández is the editor-in-chief of REC: Interventional Cardiology. F. Alfonso, and J. Sanchis are associate editors of REC: Interventional Cardiology; the journal’s editorial procedure to ensure impartial handling of the manuscript has been followed.
WHAT IS KNOWN ABOUT THE TOPIC?
- In intermediate LMCA stenoses (25% to 60% diameter) the use of invasive (ultrasound or optical coherence tomography) or functional imaging modalities (by measuring the FFR) has been proposed to eventually indicate the need for revascularization. Patients with LMCA stenoses were excluded from randomized clinical trials that assessed the prognostic capabilities of the functional assessment using the FFR.3 However, its use has been backed by several non-randomized clinical trials that confirmed that values > 0.80 are indicative of a low risk of events if revascularization is eventually spared. The iFR is a new physiological index that does not require hyperemia to be determined, which simplifies the whole process. There are still no data on the concordance between both indices in LMCA lesions or the safety of this new index in the assessment of these patients.
WHAT DOES THIS STUDY ADD?
- The iLITRO-EPIC07 trial is an attempt to prospectively assess the concordance between the FFR and the iFR, as well as the safety profile of an iFR-guided revascularization strategy.
REFERENCES
1. Lindstaedt M, Spiecker M, Perings C, et al. How good are experienced interventional cardiologist at predicting the functional significance of intermediate or equivocal left main coronary stenosis?Int J Cardiol. 2007;120:254-261.
2. Windecker S, Kohl P, Alfonso F, et al. 2014 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2014;35:2541-2619.
3. Pijls NH, van Schaardenburgh P, Manoharan G, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis:5-year follow-up of the DEFER Study. J Am Coll Cardiol. 2007;49:2105-2111.
4. Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve vs. angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213-224.
5. De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI vs. medical therapy in stable coronary disease. N Engl J Med. 2012;367:991-1001.
6. Hamilos M, Muller O, Cuisset T, et al. Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation. 2009;120:1505-1512.
7. Sen S, Escaned J, Malik IS, et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis:results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J Am Coll Cardiol. 2012;59:1392-1402.
8. Davies JE, Sen S, Dehbi HM, et al. Use of the instantaneous wave-free ratio or fractional flow reserve in PCI. N Engl J Med. 2017;376:1824-1834.
9. Götberg M, Christiansen EH, Gudmundsdottir IJ, et al. iFRSWEDEHEART Investigators. Instantaneous free-wave ratio versus fractional flow reserve to guide PCI. N Engl J Med. 2017;376:1813-1823.
10. Warisawa T, Cook CM, Rajkumar C, et al. Safety of Revascularization Deferral of Left Main Stenosis Based on Instantaneous Wave-Free Ratio Evaluation. JACC Cardiovasc Interv. 2020;13:1655-1664.
11. Kobayashi Y, Johnoson NP, Berry C, et al. The influence of lesion location on the diagnostic accuracy of adenosine-free coronary pressure wire measurements. J Am Coll Cardiol Interv. 2016;9:2390-2399.
12. de la Torre Hernandez JM, Hernandez F, Alfonso F, et al. Prospective application of pre-defined intravascular ultrasound criteria for assessment of intermediate left main coronary artery lesions results from the multicenter LITRO study. J Am Coll Cardiol. 2011;58:351-358.
13. Nair PK, Marroquin OC, Mulukutla SR, et al. Clinical utility of regadenoson for assessing fractional flow reserve. JACC Cardiovasc Interv. 2011;1085-1092.
14. Ragosta M, Dee S, Sarembock IJ, et al. Prevalence of unfavorable angiographic characteristics for percutaneous intervention in patients with unprotected left main coronary artery disease. Catheter Cardiovasc Interv. 2006;68:357-362.
15. Cameron A, Kemp HG Jr, Fisher LD, et al. Left main coronary artery stenosis:angiographic determination. Circulation. 1983;68:484-489.
16. Fisher LD, Judkins MP, Lesperance J, et al. Reproducibility of coronary arteriographic reading in the coronary artery study (CASS). Catheter Cardiovasc Diagn. 1982;8:565-575.
17. Arnett EN, Isner JM, Redwood DR, et al. Coronary artery narrowing in coronary heart disease:comparison of cineangiographic and necropsy findings. Ann Intern Med. 1979;91:350-356.
18. Lenzen MJ, Boersma E, Bertrand ME, et al. Management and outcome of patients with established coronary artery disease:the Euro Heart Survey on coronary revascularization. Eur Heart J. 2005;26:1169-1179.
19. Kandzari DE, Colombo A, Park SJ, et al. Revascularization for unprotected left main disease:evolution of the evidence basis to redefine treatments standards. J Am Coll Cardiol. 2009;54:1576-1588.
20. Botman CJ, Schonberger J, Koolen S, et al. Does stenosis severity of native vessels influence bypass graft patency?A prospective FFR-guided study. Ann Thorac Surg. 2007;83:2093-2097.
21. Mallidi J, Atreya AR, Cook J, et al. Long term outcomes following fractional flow reserve guided treatment of angiographically ambiguous left main coronary artery disease:a meta-analysis of prospective cohort studies. Catheter Cardiovasc Interv. 2015;86:12-18.
22. Petraco R, van de Hoef TP, Nijjer S, et al. Baseline instantaneous wave-free ratio as a pressure-only estimation of underlying coronary flow reserve:results of the JUSTIFY-CFR Study (Joined Coronary Pressure and Flow Analysis to Determine Diagnostic Characteristics of Basal and Hyperemic Indices of Functional Lesion Severity Coronary Flow Reserve). Circ Cardiovasc Interv. 2014;7:492-502.
23. Nijjer SS, de Waard GA, Sen S, et al. Coronary pressure and flow relationships in humans:phasic analysis of normal and pathological vessels and the implications for stenosis assessment:a report from the Iberian-Dutch-English (IDEAL) collaborators. Eur Heart J. 2016;37:2069-2080.
24. Lee JM, Shin ES, Nam CW, et al. Clinical outcomes according to fractional flow reserve or instantaneous wave-free ratio in deferred lesions. JACC Cardiovasc Interv. 2017;10:2502-2510.
Corresponding author: Unitat Cardiologia Intervencionista, Hospital Germans Trias i Pujol, Carretera de Canyet SN, 08916 Badalona, Barcelona, Spain
E-mail address: oriolrodriguez@gmail.com (O. Rodríguez-Leor).