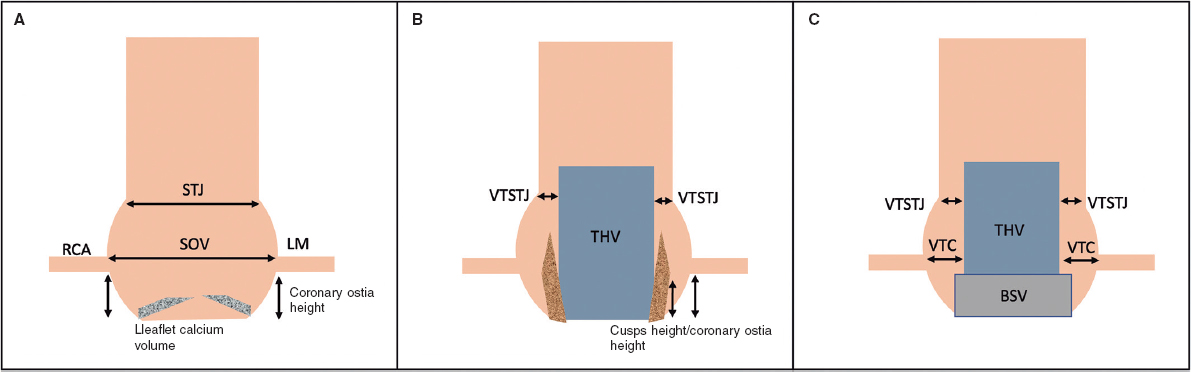
CASE PRESENTATION
Eighty-two year-old-woman with a past medical history of high blood pressure, dyslipidemia, primary hypothyroidism, iron deficiency anemia, chronic renal disease, a glomerular filtration rate of 52 mL/min, an episode of ischemic colitis resolved using conservative therapy 2 years ago and documented peripheral arterial disease with carotid artery atheromatous plaque without significant stenosis.
The patient showed long-term degenerative aortic valve disease with double aortic lesion with severe stenosis (mean flow velocity, 4.1 m/s; mean gradient, 42 mmHg; valve area, 0.98 cm2) and mild-to-moderate regurgitation, with preserved left ventricular ejection fraction, and symptomatic in class II of the New York Heart Association for dyspnea. The patient complained of episodes of non-exertional angina for which she required several hospital admissions over the last few months.
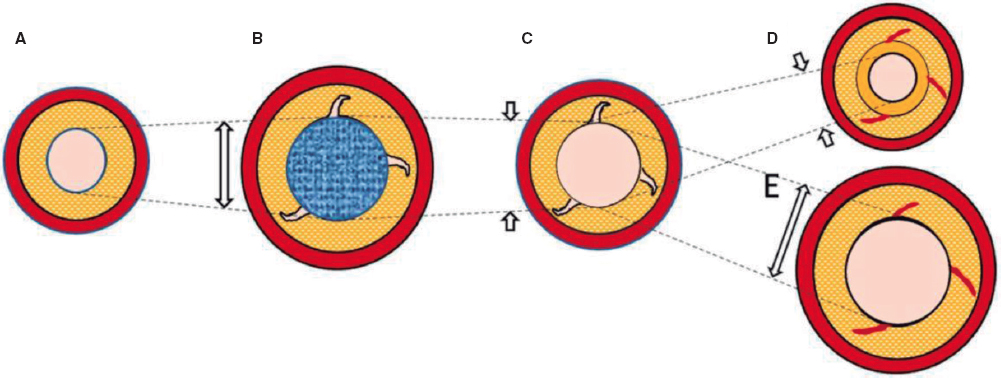
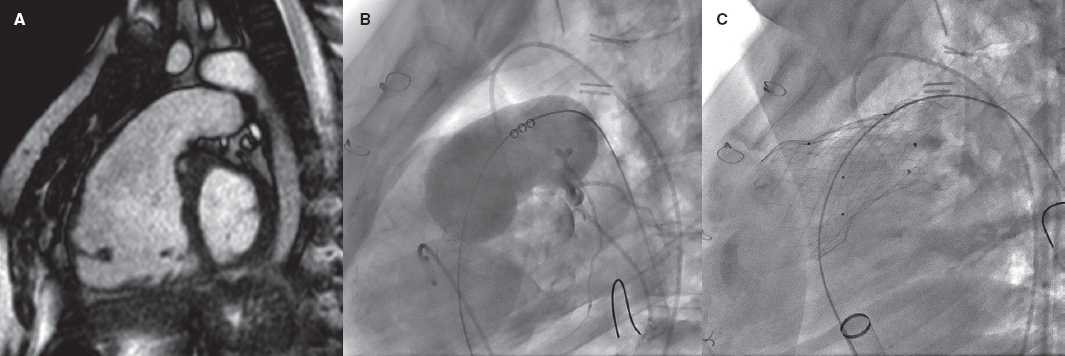
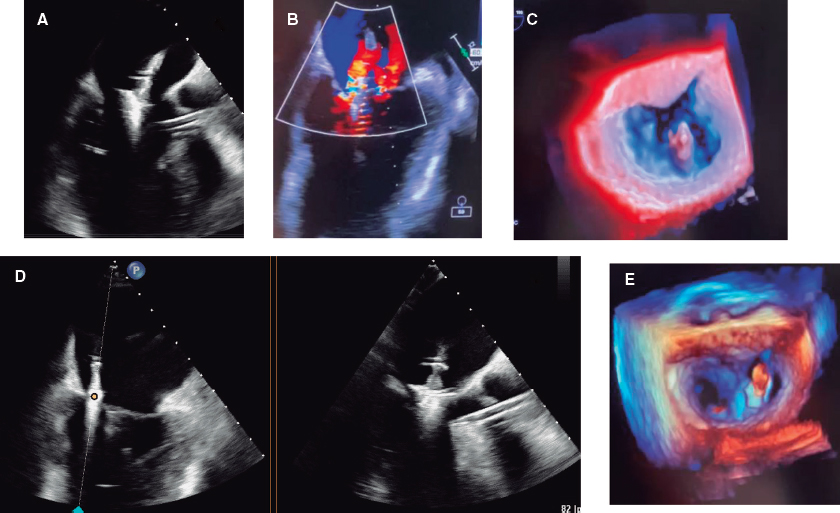
The coronary angiography revealed coronary artery disease of the left main coronary artery and 2 vessels: calcified and elongated left main coronary artery with a borderline significant distal lesion affecting the bifurcation with the anterior descending coronary artery, 2 ramus medianus and the circumflex coronary artery; the anterior descending coronary artery with a severely calcified ostial lesion, first and second ramus medianus with significant calcified ostial lesions, and circumflex coronary artery with a moderate ostial lesion (figure 1, figure 2 and video 1 of the supplementary data) with a narrow-caliber and short distal vessel. The aortogram showed a calcified tricuspid aortic valve with limited opening of the leaflets and mild aortic regurgitation and nondilated aortic regurgitation root and ascending aorta without significant atheromatosis (figure 3 and video 2 of the supplementary data). The arteriography of the lower limbs showed a non-calcified, non-tortuous iliac-femoral axis with a minimum diameter of 7.3 mm in the right common femoral artery and a minimum diameter of 7.7 mm in the left common femoral artery. The short-term risk according to the Society of Thoracic Surgeons was 10.79%.
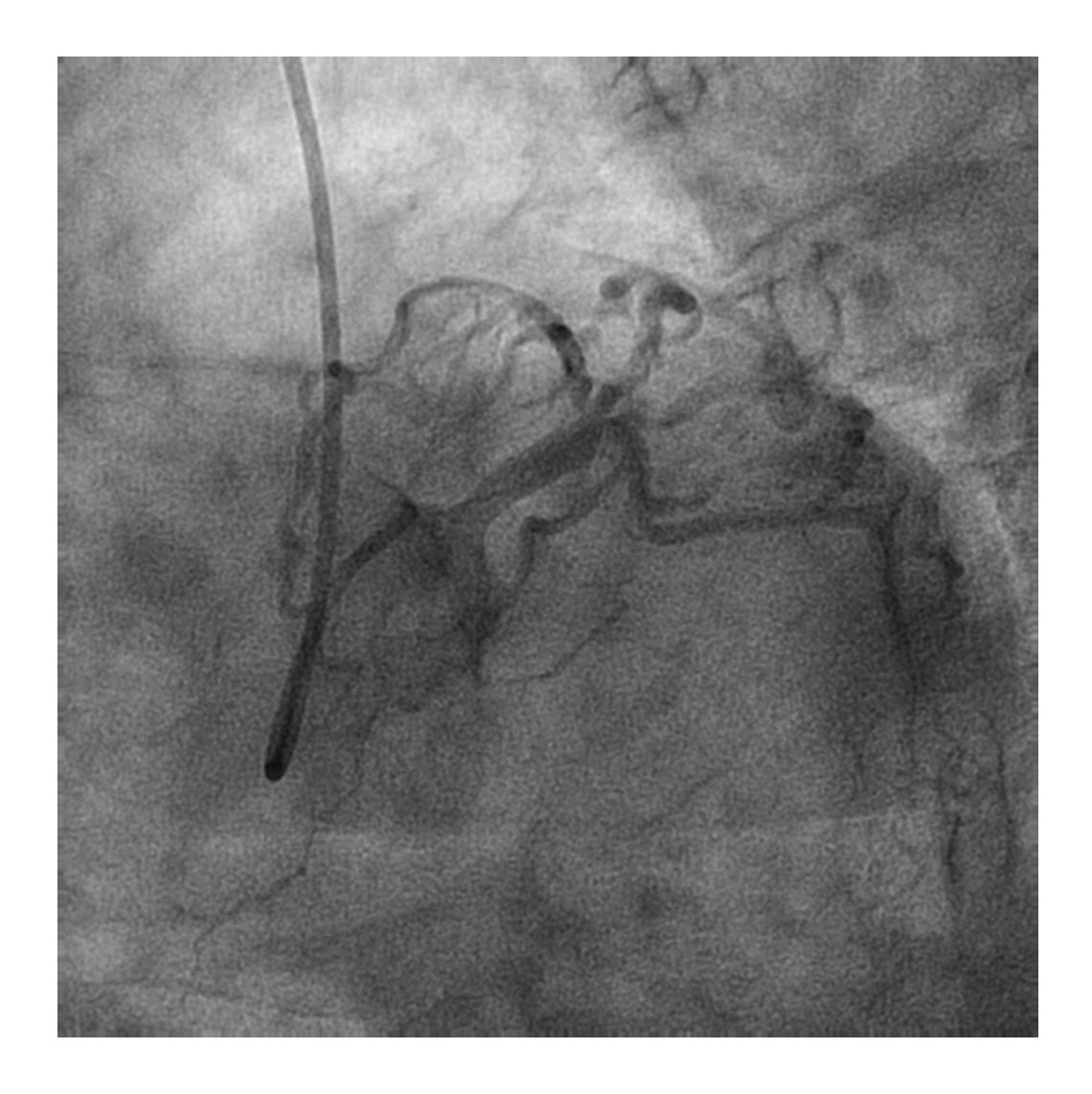
Figure 1. Coronary angiography in caudal left-anterior-oblique view showing significant distal left main coronary artery disease with damage to the anterior descending coronary artery and two intermediate branches.
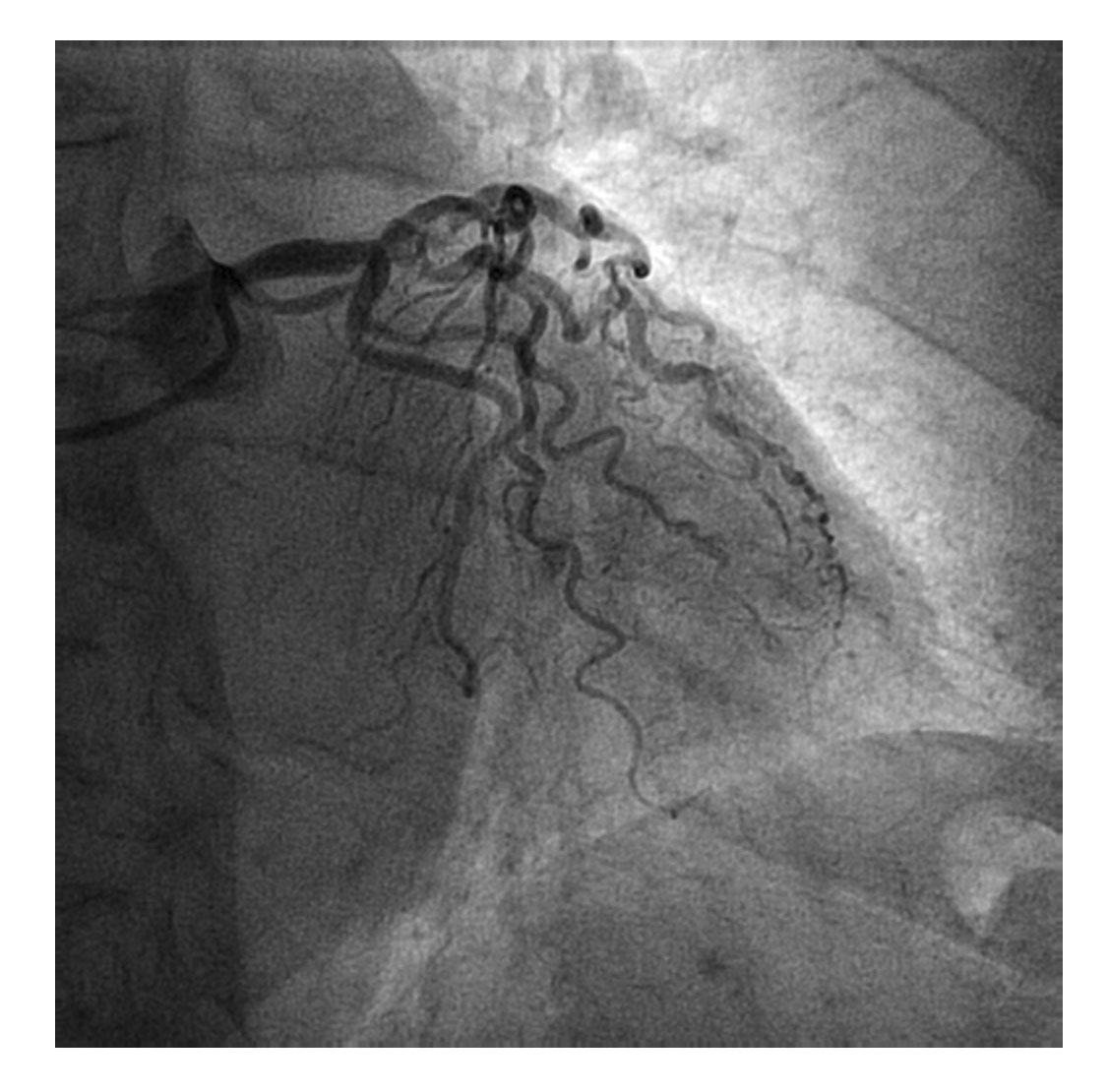
Figure 2. Coronary angiography in caudal right-anterior-oblique view.
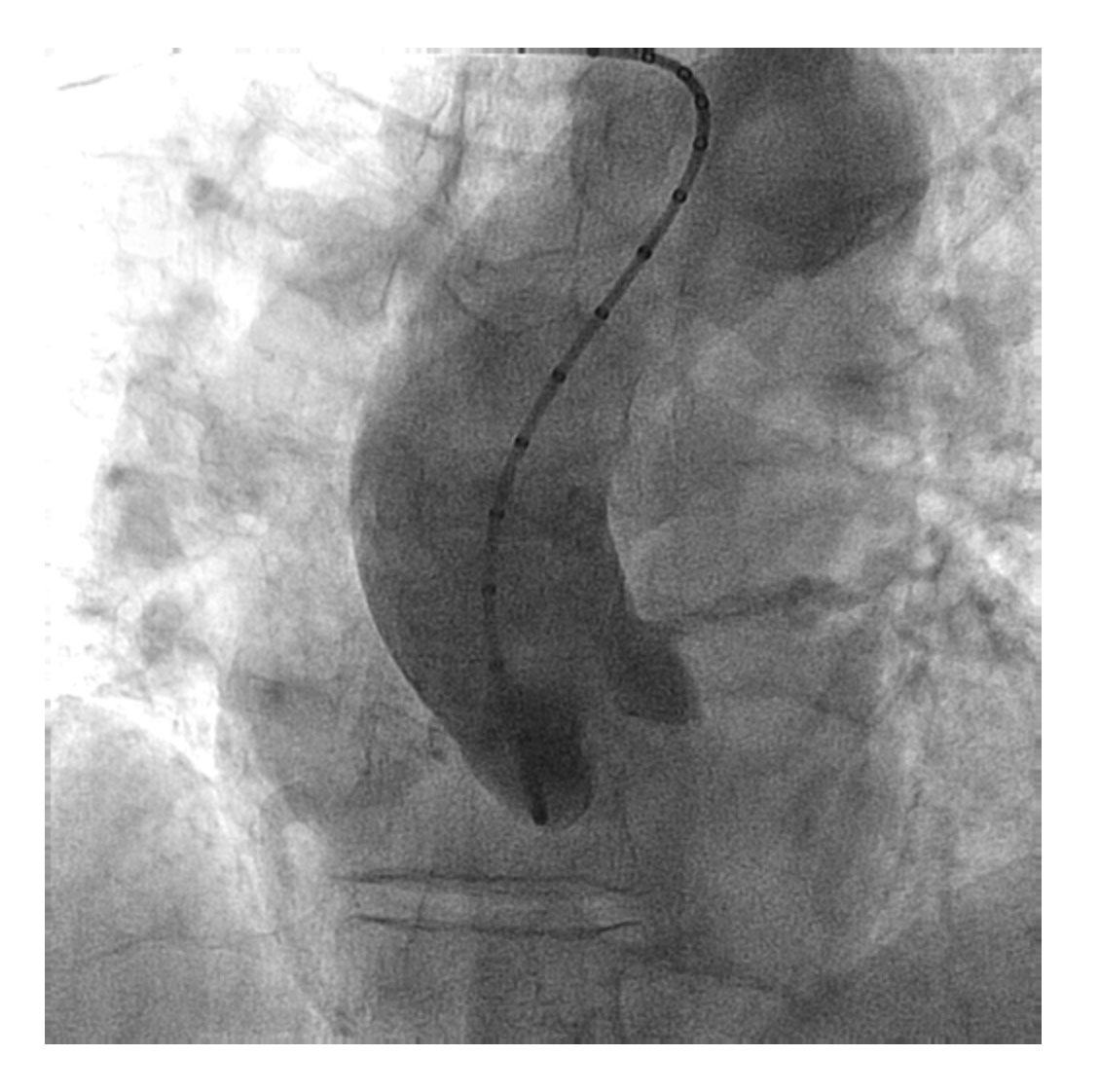
Figure 3. Aortogram showing one tricuspid aortic valve with moderate calcification of the leaflets, nondilated aortic root and ascending aorta without significant atheromatosis.
SUPPLEMENTARY DATA
Corresponding author: Instituto del Corazón, Hospital Germans Trias i Pujol, Carretera Canyet s/n, 08916 Badalona, Barcelona, Spain.
E-mail address: beatriztoledanoleon@gmail.com (B. Toledano).