A 48-year-old woman with congenital pulmonary stenosis who required surgical valvuloplasty in 1978 presented with progressive dyspnea. The cardiovascular magnetic resonance imaging performed confirmed the presence of dilated right ventricle, severe regurgitation, and pulmonary artery aneurysm (39 × 25 mm). The heart team decided to perform a transcatheter pulmonary valve implantation. During pre-stenting with an uncovered 15-25 mm × 47-55 mm CP Stent (NuMED, United States) mounted on a 25 mm balloon of the native right ventricular outflow tract, stent embolization with spontaneous anchoring to the left pulmonary artery occurred (video 1 of the supplementary data, and figure 1A). Since the patient remained stable, a wait-and-see approach was decided to facilitate stent endothelialization. The stent (figure 1B) was used as the anchoring substrate 2 months apart of the proximal implantation for 2 longer Andrastent XXL 57 mm-stents (Andramed, Germany) on a 30 × 40 mm XL AndraBalloon to create a landing zone for the 29 mm Sapien-3 valve. The rest of the procedure was successful (figure 1C). The patient remained asymptomatic, with no perfusion defects as confirmed by the ventilation/perfusion lung scan and a mean transvalvular gradient of 7 mmHg without any residual regurgitation at the 6-month follow-up (figure 1D).
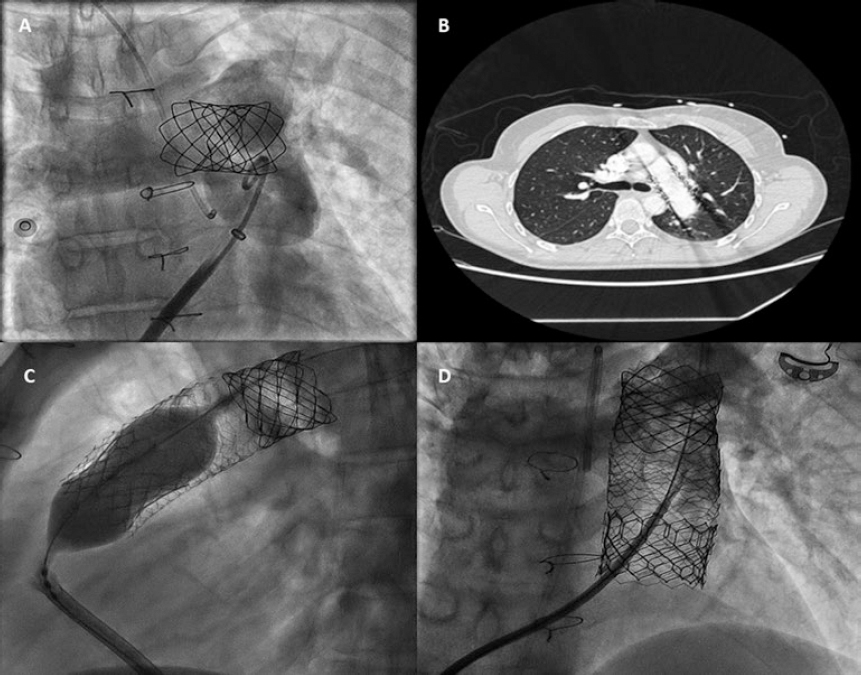
Figure 1.
In cases of aneurysmal pulmonary trunk and dilated native/non-calcified right ventricular outflow tract, the high risk of stent or valve migration may be prevented by the “planned” implantation of a first stent of smaller dimensions in a pulmonary branch. Then, sequential proximal stents may be anchored to this landing zone, which facilitates the reconstruction of pulmonary trunk with low risk of flow compromise in the jailed pulmonary branch. Further studies to assess this scenario are warranted.
CONFLICTS OF INTEREST
J.L. Zunzunegui is a proctor for Edwards Lifesciences.
SUPPLEMENTARY DATA
Video 1. Aparisi A. DOI: 10.24875/RECICE.M19000088
Corresponding author: Instituto de Ciencias del Corazón (ICICOR), Hospital Clínico Universitario de Valladolid, Ramón y Cajal 3, 47005 Valladolid, Spain.
E-mail address: ijamat@gmail.com (I.J. Amat-Santos).











