ABSTRACT
The primary endpoint of the ISCHEMIA trial, whose results were presented at the American Heart Association congress back in 2019, was to determine whether an initial invasive strategy of cardiac catheterization and successful revascularization plus optimal medical treatment would reduce the primary composite endpoint of cardiovascular death or myocardial infarction in patients with chronic coronary syndrome compared to an initial conservative strategy of optimal medical treatment. Out of 5179 patients, 2588 were randomized to receive an invasive strategy and 2591 to receive conservative strategy. At the 4-year follow-up, the primary endpoint showed no significant differences between both groups revolutionizing mass media. In our opinion, we should be cautious when interpreting the results of a study that has not been published yet. There is no doubt, however, that the ISCHEMIA trial deals with an important matter, that the most powerful medical treatment was able to modify the natural history of this disease in patients with chronic coronary syndrome.
Keywords: Chronic coronary syndrome. Conservative strategy. Invasive strategy.
RESUMEN
El estudio ISCHEMIA, cuyos resultados se presentaron en el congreso de la American Heart Association en 2019, tiene como objetivo principal determinar si una estrategia invasiva inicial de cateterización cardiaca y revascularización exitosa, junto con el tratamiento médico óptimo, reduce el objetivo primario combinado de muerte cardiovascular o infarto de miocardio en pacientes con síndrome coronario crónico, en comparación con una estrategia conservadora inicial de tratamiento médico óptimo. De 5.179 pacientes, se aleatorizaron 2.588 para seguir una estrategia invasiva y 2.591 para una estrategia conservadora. A los 4 años de seguimiento, el objetivo primario no mostró diferencias significativas entre ambos grupos, lo que generó un gran revuelo mediático. En nuestra opinión, debemos ser prudentes al interpretar los resultados de un estudio aún sin publicar. No obstante, es innegable que el estudio ISCHEMIA aborda la importante cuestión de que el tratamiento médico más potente en pacientes con síndrome coronario crónico ha demostrado modificar la evolución natural de la enfermedad.
Palabras clave: Estrategia conservadora. Estrategia invasiva. Síndrome coronario crónico.
Abbreviations: CCS: chronic coronary syndrome. CS: conservative strategy. IS: invasive strategy. OMT: optimal medical treatment. PCI: percutaneous coronary intervention.
INTRODUCTION
According to current recommendations of the clinical practice guidelines for the management of patients with chronic coronary syndromes (CCS), the optimal medical treatment (OMT) is a fundamental therapy to improve symptoms, reduce the progression of atherosclerosis, and prevent the occurrence of atherothrombotic events. Coronary revascularization has a significant role in the management of these patients as an adjuvant therapy of OMT. Similarly, traditional studies have proven that symptoms subside, and prognosis improves.1-3 However, current studies question the benefits of routine revascularization in patients with CCS because of the similar mortality and myocardial infarction rates seen in patients who received OMT with and without percutaneous coronary intervention (PCI) in the COURAGE clinical trial;4 and with and without PCI or surgical coronary revascularization in the BARI 2D trial.5 These studies share common characteristics that the researchers of the ISCHEMIA trial (NCT01471522) have taken into account when designing their study: a) there is a selection bias in both studies since randomization takes place after knowing coronary anatomy; b) among the inclusion criteria no minimal threshold of myocardial ischemia is required; and c) only covered stents were used in a very small number of patients.
STUDY DESIGN AND ENDPOINTS
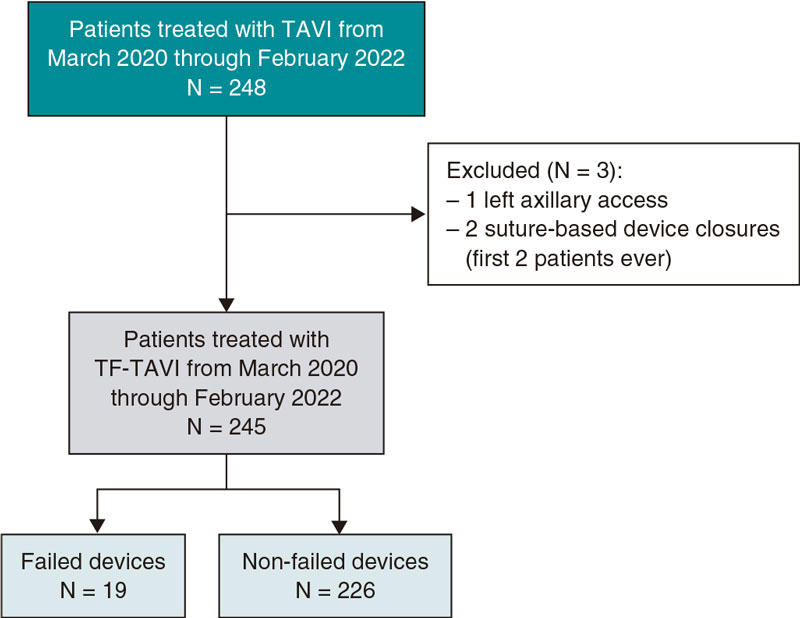
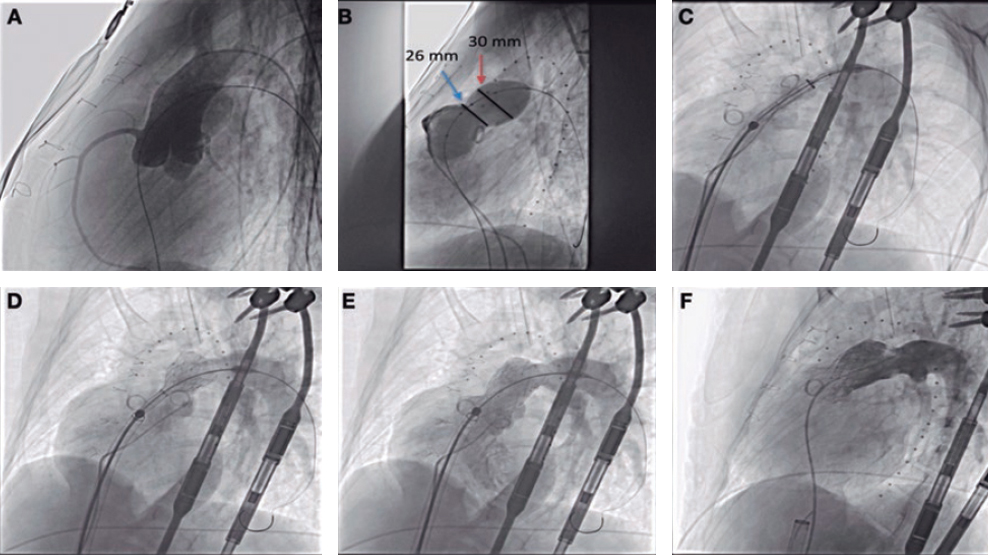
The ISCHEMIA trial original primary endpoint was to determine whether an initial invasive strategy (IS) of cardiac catheterization and successful revascularization (with PCI or surgical revascularization) plus OMT would reduce the composite primary endpoint of cardiovascular death or myocardial infarction in patients with CCS and moderate or severe ischemia (with medically controllable or absent symptoms) compared to an initial conservative strategy (CS) of OMT, with catheterization spared for cases where OMT failed (figure 1). Secondary endpoints were cardiovascular death or myocardial infarction and objectives of quality of life. The study was initiated back in 2012 but, in June 2017, an independent panel of experts from the National Heart, Lung, and Blood Institute (NHLBI) changed the study double primary endpoint for a composite endpoint of 5 variables: cardiovascular death, myocardial infarction, resuscitated cardiac arrest, and unstable angina or heart failure related hospitalization.6 Median follow-up was 3.3 years.
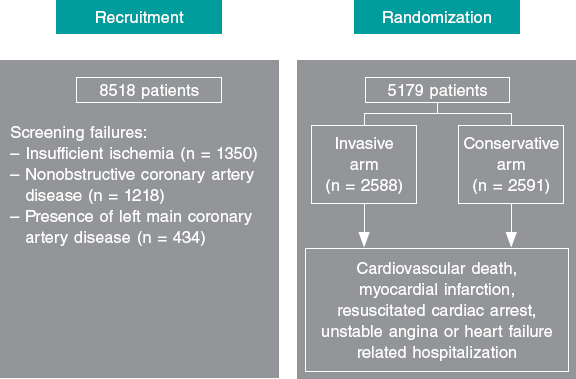
Figure 1. Flow of patients from inclusion until randomization.
The most interesting aspects of the study design are:
- The degree of ischemia to assess whether a patient met the study requirements was established according to predefined criteria through one of the following additional studies: nuclear medicine test, stress echocardiogram, cardiac magnetic resonance or ergometry.
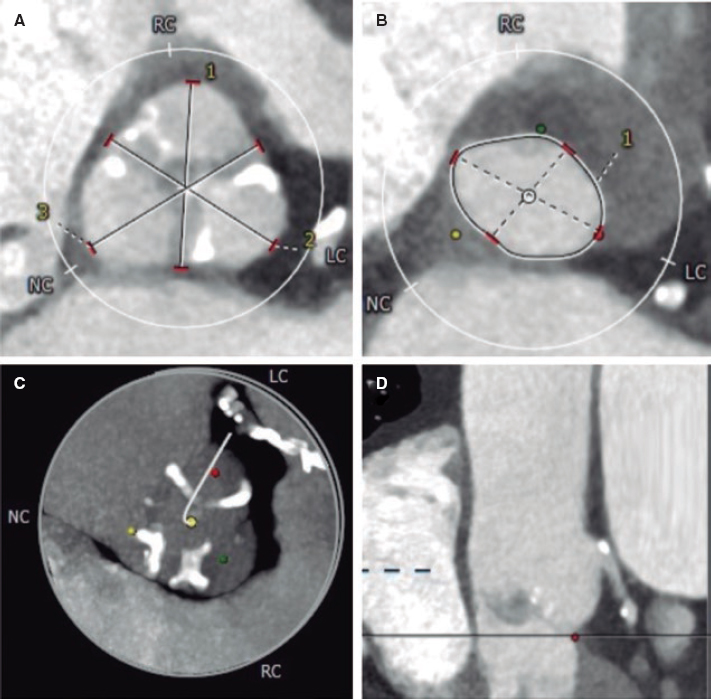
- The main exclusion criteria were the presence of recent heart failure, acute coronary syndrome or revascularization, left ventricle ejection fraction < 35%, left main coronary artery stenosis > 50% (the study required a computed tomography [CT] scan prior to randomization) or the presence of unstable angina at the beginning of the study despite maximal medical treatment.
RESULTS
Of a total of 8518 patients screened, 5179 were randomized to receive an IS (n = 2588) or CS (n = 2591) with a median follow-up of 3.3 years (figure 1). The baseline characteristics between both groups did not vary significantly.7,8 Mean age was 64 years old and 23% of the patients recruited were women. The mean ejection fraction was 60%. In 75% of the patients ischemia imaging test was used while ergometry was used in the remaining 25%. A core laboratory determined that 54% of randomized patients had severe ischemia, 33% moderate ischemia, 12% mild or no ischemia, and 1% ischemia that could not be interpreted. Eighty percent of the patients of the IS arm were revascularized; 74% with PCI and the remaining ones with coronary revascularization surgery. Two thirds of the non-revascularized patients had significant coronary artery disease, and one third nonrevascularizable extensive coronary artery disease.
The study met its 4-year primary endpoint in 15.5% and 13.6% of the patients from the CS and IS group, respectively without any significant differences (adjusted hazard ratio [HR], 0.93 [0.8-1.08]; P = .34). There was a tendency towards a higher rate of events within the first 6 months in the IS arm that reversed in favor of such arm at the 2-year follow-up. Regarding myocardial infarction, the spontaneous one was reduced in the IS arm (adjusted HR, 0.67 [0.53-0.83]; P < .01) while the perioperative infarction was increased in this arm (adjusted HR, 2.98 [1.87-4.74]; P < .01).
COMMENT
The ISCHEMIA trial was presented in 3 late-breaking clinical trial sessions held in Philadelphia by the American Heart Association congress back in November 2019: clinical outcomes, objectives of quality of life, and results in patients with end-stage renal disease.7 Ever since, the media has made a big deal out of it9 by reporting on the preoccupation of different associations of patients following a message delivered on the news: «thousands of patients are receiving unnecessary procedures».
In our opinion, we should be cautious when interpreting the results of a popular study that still unpublished. What is undeniable—and researchers should take credit for it—is that the ISCHEMIA trial discussed an important issue: the management of patients with stable coronary artery disease (now called CCS) with the most powerful medical treatment that was able to modify the natural history of this disease.
There are 4 main issues we should take away from this study.
- It was a very difficult study to conduct where the recruitment of patients was slow in most participant centers. Before reaching 50% of the events estimated for the study primary endpoint, such primary endpoint had to be changed to increase the number of events, which is a non-desirable practice when designing a study.10.
- Inclusion criteria were very rigorous. To recruit a patient the presence of coronary artery disease had to be confirmed through a CT scan (anatomical study) followed by the presence of significant ischemia (functional study, 50% of randomized patients through nuclear medicine test), something rare in the management of these patients in our setting.
- On the other hand, the ISCHEMIA was a trial on the management of patients with stable coronary artery disease, not on revascularization vs no revascularization as it was announced by the media at one point. This is very clear if we consider the following data: only 80% of the patients from the IS group were revascularized and up to 23% of those assigned to the CS group were revascularized. The ISCHEMIA was not a PCI trial either since only 74% of the patients revascularized were treated with this technique while coronary revascularization surgery was performed in the remaining cases. This means that 1 in 5 patients from the IS group was not revascularized, but 1 in 4 patients from the CS group was.
- The study main results confirm that when both strategies are compared there are similar risks of presenting the composite endpoint of cardiovascular death, myocardial infarction, resuscitated cardiac arrest and unstable angina or heart failure related hospitalization. Analyzing the remaining study endpoints, it can be said that the CS has a lower risk of perioperative myocardial infarction (for obvious reasons) or heart failure related hospitalization. However, the initial invasive strategy has a lower risk of spontaneous myocardial infarction and unstable angina related hospitalization, and is associated with an undeniable symptomatic relief and improved quality of life in patients with angina symptoms. On the analysis of adverse events, it is obvious that perioperative myocardial infarction does not have the same prognostic value as spontaneous myocardial infarction. Also, the spontaneous myocardial infarction curves and primary assessment criterion vary at the end of the follow-up. This favors the revascularization strategy yet despite the great deal of patients of the CS group who were revascularized, meaning that it will important to see the long-term results.
In conclusion, the ISCHEMIA is a historic clinical trial that reinstates the importance of aggressive medical treatment in patients with stable coronary artery disease. However, before claiming victory against revascularization the improved quality of life provided by revascularization and the inherent limitations of an unpublished study, some of which have already been discussed, should not be forgotten.
CONFLICTS OF INTEREST
None reported.
REFERENCES
1. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41: 407-477.
2. Fleg JL, Forman DE, Berra K, et al. Secondary prevention of atherosclerotic cardiovascular disease in older adults:a scientific statement from the American Heart Association. Circulation. 2013;128:2422-2446.
3. Hachamovitch R, Rozanski A, Shaw LJ, et al. Impact of ischaemia and scar on the therapeutic benefit derived from myocardial revascularization vs. medical therapy among patients undergoing stress-rest myocardial perfusion scintigraphy. Eur Heart J. 2011;32:1012-1024.
4. Boden WE, O'Rourke RA, Teo KK, et al.;COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503-1516.
5. BARI 2D Study Group. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009;360:2503-2515.
6. ISCHEMIA Trial Research Group, Maron DJ, Hochman JS, et al. International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial:Rationale and design. Am Heart J. 2018;201:124-135.
7. American Heart Association. International Study of Comparative Health Effectiveness With Medical and Invasive Approaches (ISCHEMIA). Disponible en:https://professional.heart.org/professional/ScienceNews/UCM_505226_ISCHEMIA-Clinical-Trial-Details.jsp. Consulted 20 Jan 2020.
8. Hochman JS, Reynolds HR, Bangalore S, et al. Baseline Characteristics and Risk Profiles of Participants in the ISCHEMIA Randomized Clinical Trial. JAMA Cardiol. 2019;4:273-286.
9. Biondi-Zoccai G, Frati G, Romagnoli E, et al. Final results of the ISCHEMIA trial:distinguishing mass media coverage from clinical interpretation. Minerva Cardioangiol. 2019. https://doi.org/10.23736/S0026-4725.19.05106-5.
10. Maron DJ, Harrington RA, Hochman JS. Planning and Conducting the ISCHEMIA Trial. Circulation. 2018;138:1384-1386.
Corresponding author: Servicio de Cardiología, Hospital Universitario Central de Asturias. Av. Roma, 33011 Oviedo, Asturias, Spain.
E-mail address: avanzas@secardiologia.es (P. Avanzas).