CASE RESOLUTION
Given the partial opening of the stent, it was decided to proceed with an increased pressure and assess the stability of the stent.
The stent seemed to have been deployed totally outside the right coronary artery, which is why we tried to capture it using a semi- compliant balloon in order to try to drag it towards the radial artery for implantation purposes, but such a maneuver failed (figure 1). This is how we confirmed that the stent was anchored to the ostium by just a few millimeters. Initially the intravascular ultrasound was not used here to assess the location of the stent to avoid any possible moves and manipulations of the implanted stent.
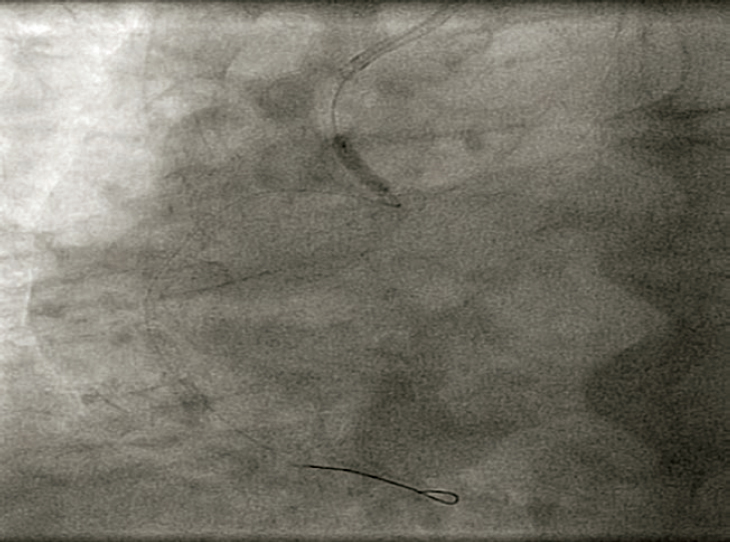
Figure 1. Attempt to drag the stent out of the coronary artery with a semi-compliant balloon.
In order to protect the stent from the deformation by the tip of guiding catheter, the Guideliner guiding catheter extension device was used (Vascular Solutions, Inc., Minneapolis, Minnesota, United States). One semi-compliant balloon of 2.5 mm in diameter was advanced towards the proximal segment of the right coronary artery where it was inflated. It was then that the Guideliner device was advanced and the inflated balloon was slightly pulled (anchoring) by placing the tip of the guiding catheter extension device into the proximal segment inside the displaced stent (figure 2).
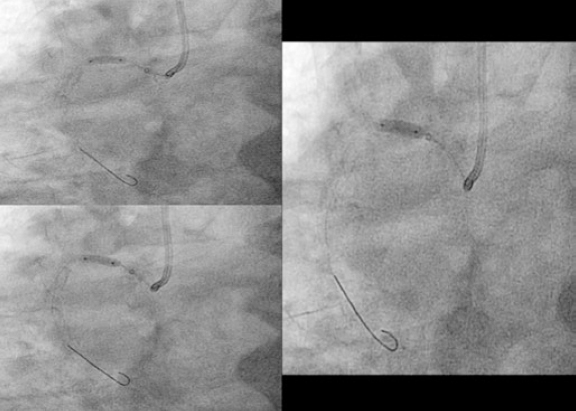
Figure 2. Advancement of the guiding catheter extension device towards the proximal segment of the right coronary artery.
Afterwards we proceeded with the eventless advancement of a new zotarolimus-coated stent (Medtronic Resolute Onyx, 4 × 22 mm) towards the proximal segment by navigating inside the guiding catheter extension device (figure 3). This second stent was implanted and anchored to the previous one and adjusted to the ostium. It was dilated with high pressure with the delivery balloon including the visible segment protruding into the aorta in order to achieve the longitudinal shortening of the stent by overexpansion (figure 4).

Figure 3. Implantation of zotarolimus-coated stent in the proximal segment of right coronary artery.
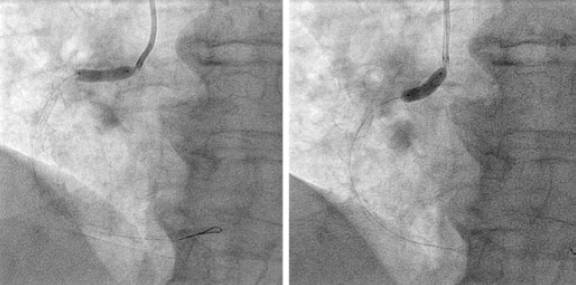
Figure 4. Post-dilatation with balloon of the previous implanted stents especially of the portion protruding into the aorta in order to achieve the greatest possible longitudinal shortening.
The angiographic results were good (figure 5A) and the intravascular ultrasound examination conducted showed the double layer of stents at ostium level with good stent apposition and expansion (figure 5B1) and the stent deployed protruding into the aorta showed wide overexpansion (figure 5B2).
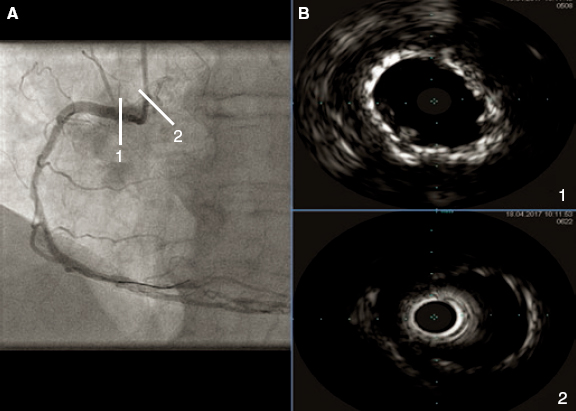
Figure 5. A: final angiographic result. B1: intracoronary ultrasound image showing the double layer of stents at ostium level with good stent apposition and expansion. B2: intracoronary ultrasound image showing the stent implanted in the first place, protruding into the aorta, and showing wide overexpansion.
We learned that the monorail extension of the guiding catheter helped us maneuver the intracoronary devices and protect the devices already implanted, which in the case of ostial lesions can prevent the deformity and the possible longitudinal shortening of the stent induced by guiding catheters.
The most radio-opaque stents can be a good option for the management of ostial lesions because of their better angiographic visualization. In this sense, chrome-cobalt alloys and, especially, chrome-platinum alloys have higher density and radiopacity. However, the chrome- platinum platform was not selected here due to its association with longitudinal deformity, especially in ostial lesions, where repeated proximal traumas are possible with the guiding catheter.
Finally, in order to avoid stent displacements with respiration we could have asked the patient to hold his breath for a few seconds, just long enough to be able to deploy the stent. However, in the presence of agitation preventing the patient’s collaboration, as it was the case here, it is advisable to use powerful sedation or analgesia, or both, to avoid complications such as stent displacement during stent deployment or issues derived from the loss of the angioplasty guidewire.
Corresponding author: Unidad de Hemodinámica y Cardiología Intervencionista, Hospital Juan Ramón Jiménez, Ronda Norte s/n, 21005 Huelva, Spain.
E-mail addresses: jroa.garrido@gmail.com (J. Roa Garrido).











