CASE RESOLUTION
After assessment by the Heart Team and taking the patient’s age and high surgical risk into consideration, surgical treatment was discarded. The study was completed with a computed tomography angiography that confirmed that the patient was eligible for trans- catheter aortic valve implantation (TAVI) through transfemoral access (figure 1A,B).
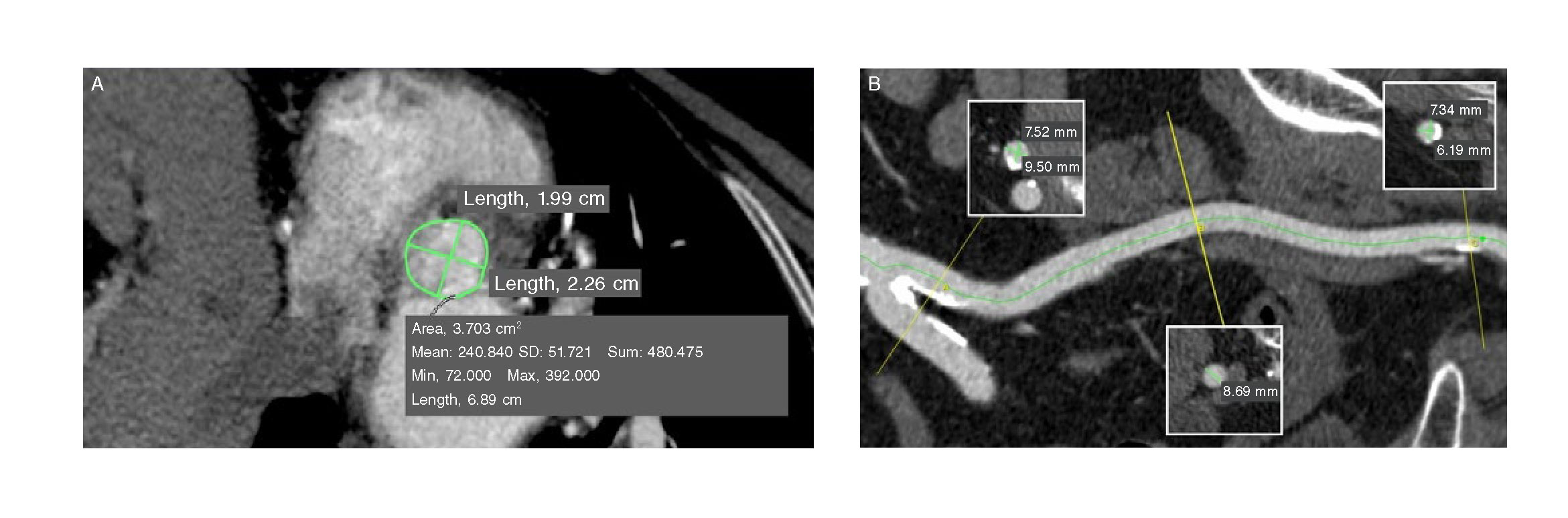
Figure 1. Computed tomography angiography prior to the procedure. A: measurements of the aortic valve ring: minimum diameter, 1.99 cm; maximum diameter, 2.26 cm; perimeter, 6.89 cm; area-derived perimeter, 3.70 cm2. B: measurements of the left iliac-femoral axis: minimum diameter of the common femoral artery, 6.19 mm; minimum diameter of the external iliac artery, 8.69 mm; minimum diameter of the primitive iliac artery, 7.52 mm. M, mean; max, maximum; min, minimum; s, sum; SD, standard deviation.
The procedure was performed under general anesthesia using the bilateral femoral access. Two 6-Fr, and 7-Fr Extra Back Up (EBU) guiding catheters were inserted into the left main coronary artery (using the “ping-pong” guiding catheter technique). Both the coronary ostia of the anterior descending coronary artery and the intermediate branches were sequentially predilated using one 2.0 mm cutting balloon (video 1 of the supplementary data) and 3 drug-eluting stents were simultaneously implanted in the anterior descending coronary artery (2.25 x 15 mm sirolimus-eluting stent), the first intermediate branch (2.25 x 18 mm zotarolimus-eluting stent), and in the second intermediate branch (2.25 x 18 mm sirolimus-eluting stent) and in this order; then we proceeded with the simultaneous inflation of the balloons (figure 2). Finally, a fourth drug-eluting stent was implanted (a 4 x 8 mm zotarolimus-eluting stent) in the left main coronary artery (figure 3 and video 2 of the supplementary data) with good results according to the optical coherence tomography (figure 4A,B). Immediately after the percutaneous coronary intervention (PCI), an expandable aortic valve with a 23 mm balloon was implanted (figure 5 and video 3 of the supplementary data) also with good results (figure 6 and video 4 of the supplementary data).
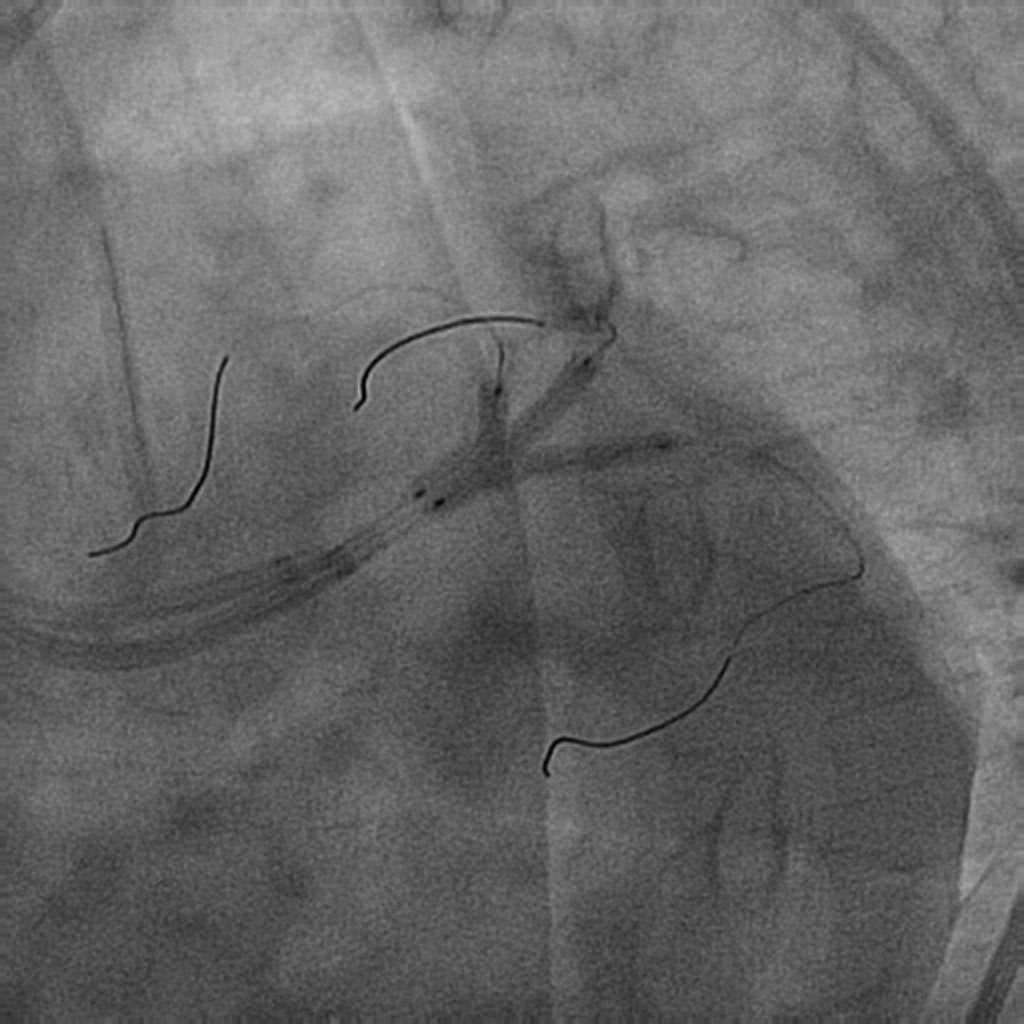
Figure 2. Simultaneous implantation of 3 drug-eluting stents in the anterior descending artery and intermediate branches.
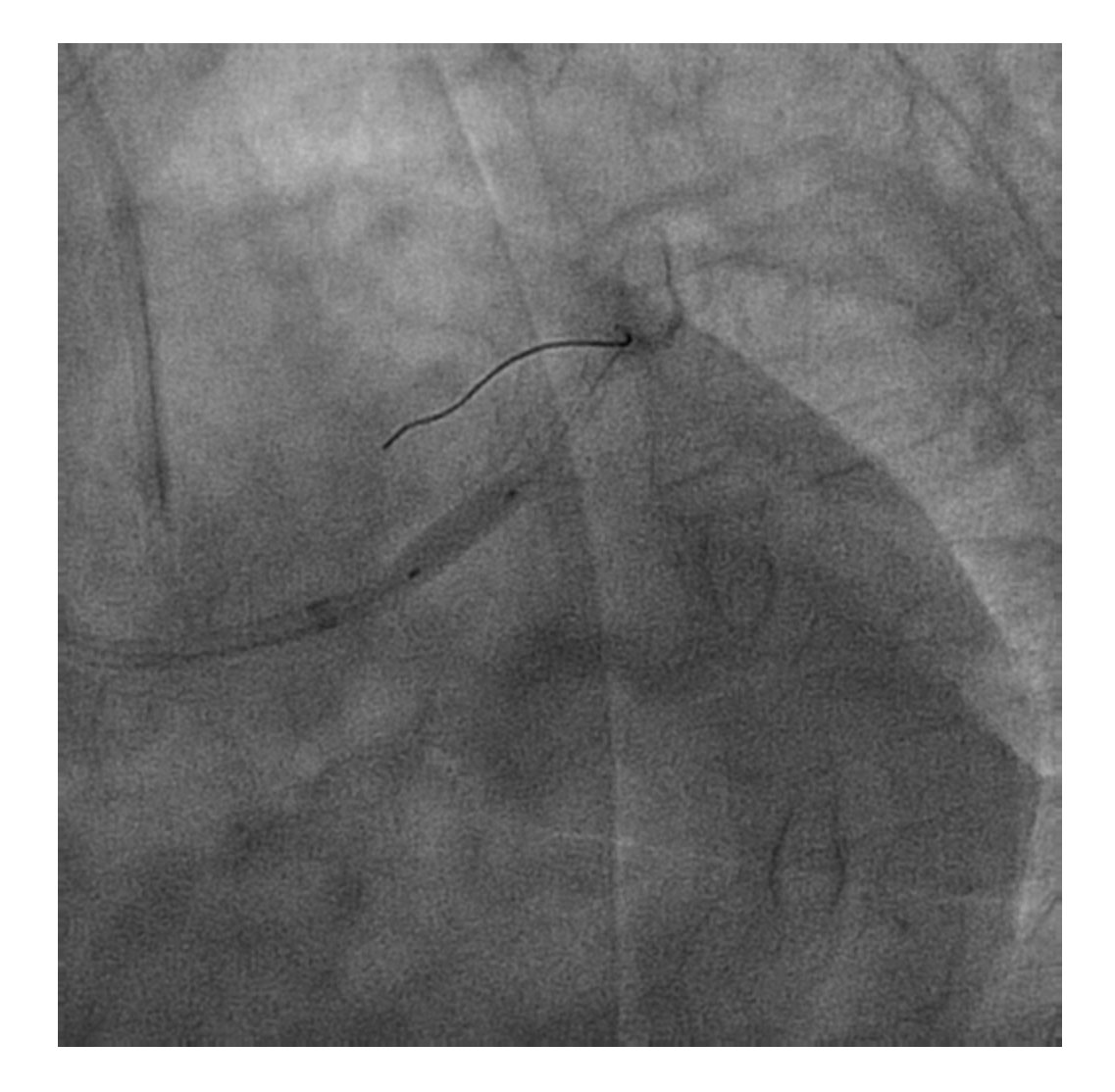
Figure 3. Implantation of a drug-eluting stent in the left main coronary artery.
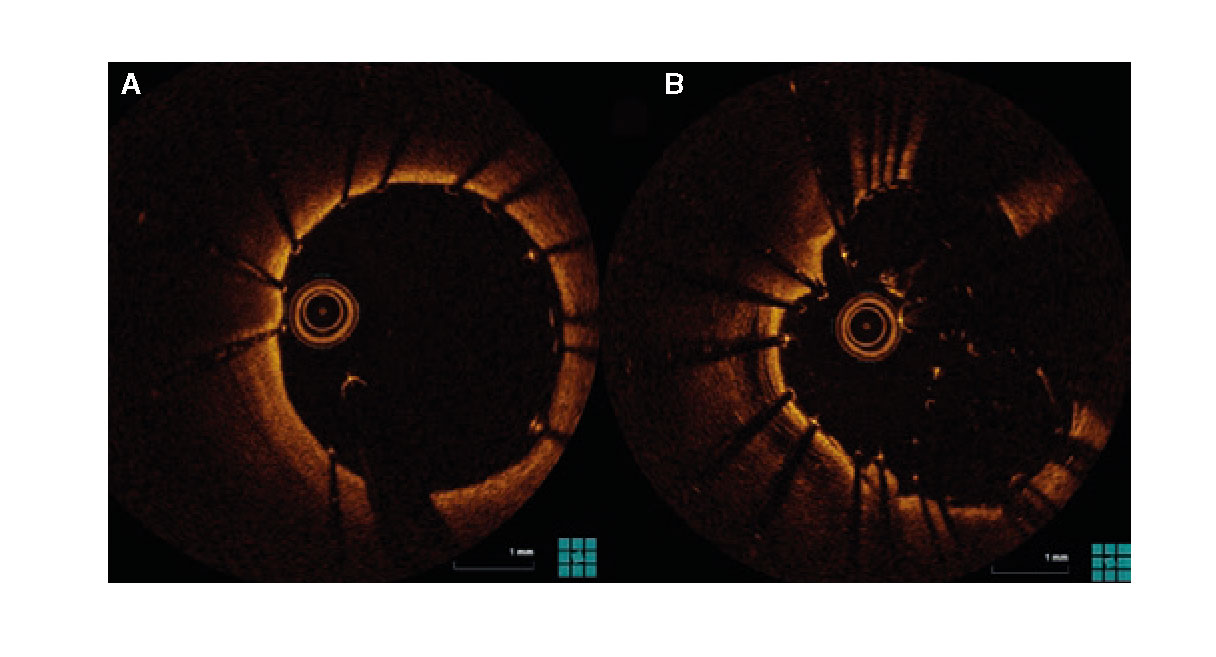
Figure 4. Optical coherence tomography after percutaneous coronary intervention. Good expansion and apposition of the drug-eluting stent in the left main coronary artery (A), and of the stents deployed in the trifurcation with adequate lumen (B).
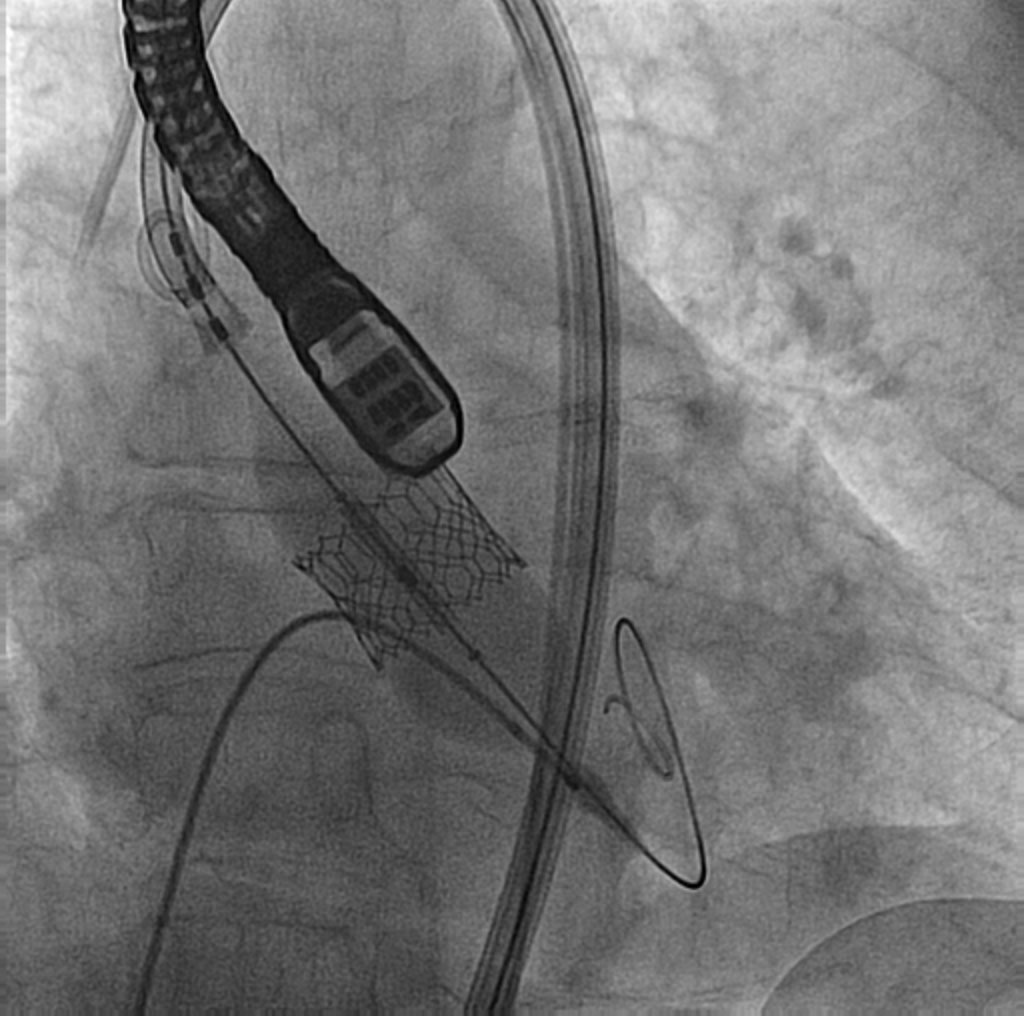
Figure 5. Implantation of an expandable aortic valve with a 23 mm balloon.
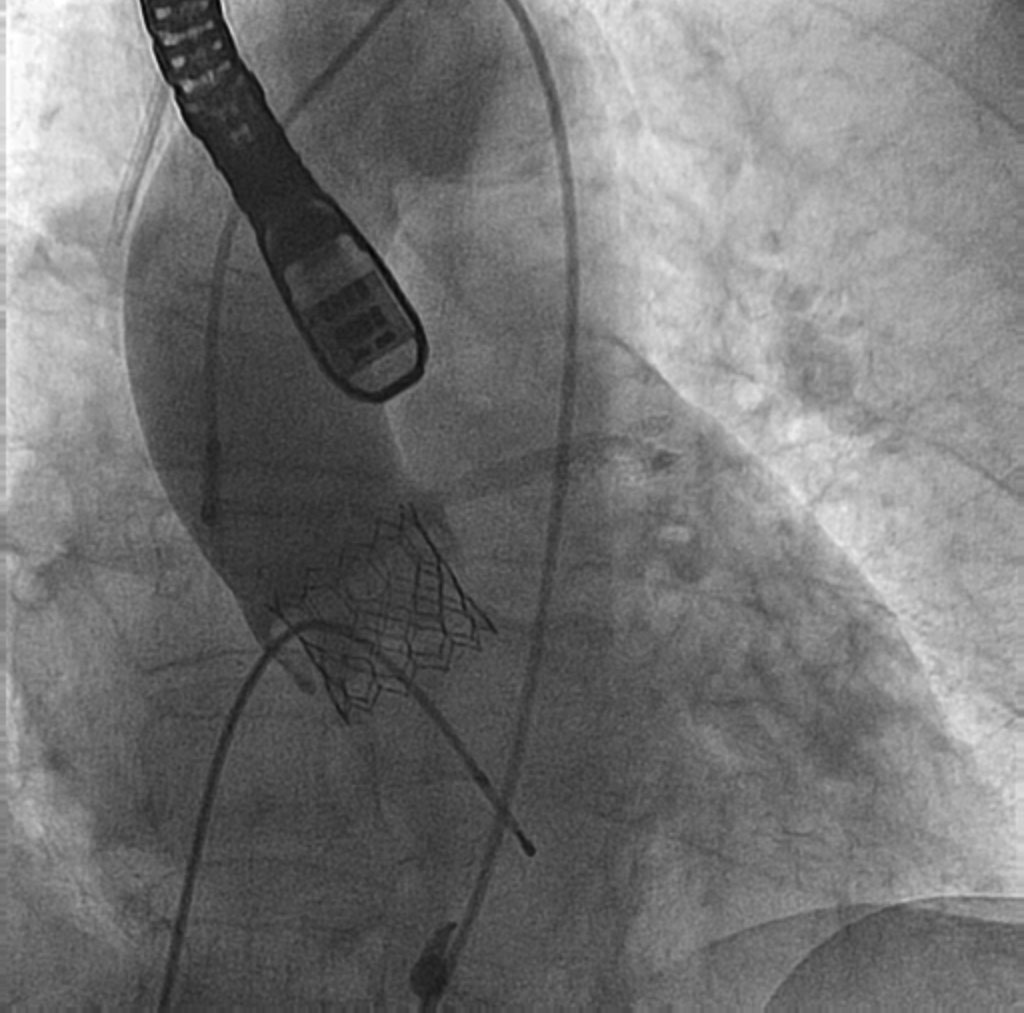
Figure 6. Final aortogram. Correct alignment of aortic valve leaflets and stents patency.
At the 28-month follow-up, the patient remained asymptomatic and with a normal functioning aortic valve.
In patients with severe aortic stenosis and left main coronary artery disease deemed to be at high surgical risk, using combined procedures (TAVI and PCI) is safe, feasible and with similar results compared to an isolated TAVI procedure.1 The combination of PCI plus TAVI on the left main coronary artery trifurcation lesion is rare.2 This case shows a safe non-surgical management of a left main coronary artery trifurcation lesion and severe aortic stenosis with good long-term results.
SUPPLEMENTARY DATA
EFERENCES
1. Chakravarty T, Sharma R, Abramowitz Y, et al. Outcomes in Patients With Transcatheter Aortic Valve Replacement and Left Main Stenting:The TAVR-LM Registry. J Am Coll Cardiol. 2016;67:951-960.
2. López U, García F, Robledo R, Fernández E, Borrego R, Morales N. Distal left main trifurcation disease in a patient with porcelain aorta. Cardiovasc Revasc Med. 2017;18:S27-S29.
Corresponding author: Instituto del Corazón, Hospital Germans Trias i Pujol, Carretera Canyet s/n, 08916 Badalona, Barcelona, Spain.
E-mail address: beatriztoledanoleon@gmail.com (B. Toledano).











