CASE PRESENTATION
This is the case of a 51-year old male without a past medical history. One month before his admission he experienced fast heart palpitations associated with diaphoresis, nausea and vomit. Both the electrocardiogram and the Holter monitor showed recurring episodes of monomorphic ventricular tachycardia (figure 1). The physical examination confirmed the presence of an aortic ejection murmur exacerbated when performing the Valsalva maneuver. The transthoracic echocardiography showed obstructive asymmetric septal hypertrophy with a 32-mm maximum septal diameter (figure 2A), a 65-mmHg gradient in the left ventricular outflow tract, and systolic anterior motion of the mitral valve with moderate regurgitation. The cardiovascular magnetic resonance imaging confirmed the presence of extensive myocardial fibrosis as a risk factor of sudden death (figure 2B and video 1 of the supplementary data). Amiodarone and propranolol were prescribed, and an automatic defibrillator was implanted as a secondary prevention measure. The patient was readmitted to the hospital 4 months later with signs of electrical storm with multiple discharges provided by the device implanted. Deep sedation, mechanical ventilation, and hemodynamic support were administered, and the stellate ganglion was blocked. However, the patient progression was poor with persistent episodes of ventricular tachycardia that triggered the mapping of cardiac electrophysiology using the CARTO 3 system (Biosense Webster, Israel). The ablation of a septal macroreentrant circuit of the left ventricle associated with the clinical ventricular tachycardia was unsuccessful (figure 2C).
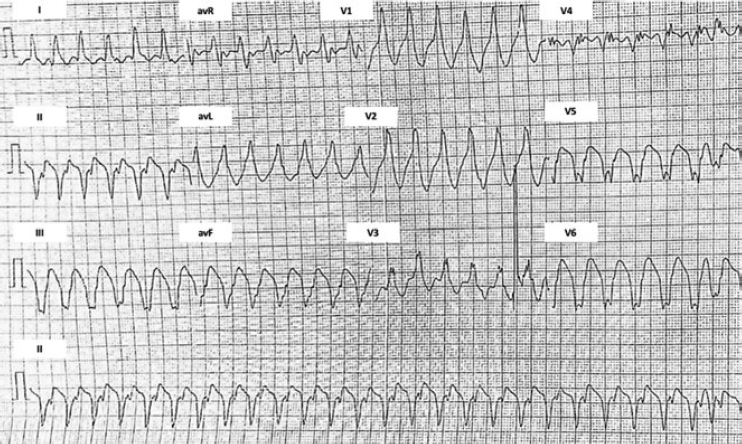
Figure 1. Initial electrocardiogram. Ventricular tachycardia originated at the mid-inferior septum of the left ventricle.
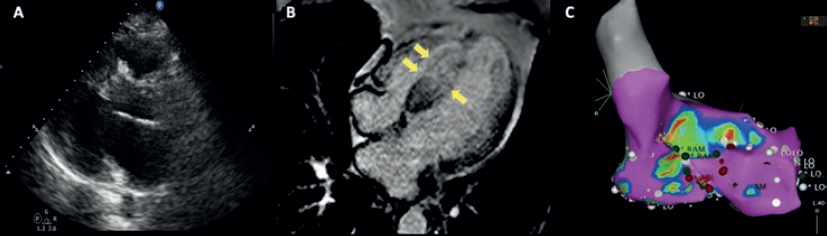
Figure 2. A: transthoracic echocardiography. Interventricular septum with a 32 mm diameter. B: magnetic resonance imaging showing late contrast (arrows). C: mapping of cardiac electrophysiology and ablation attempt of the septal macroreentrant. LO, voltage label; RAM, local electrogram label.
A bail-out alcohol septal ablation procedure was attempted that showed a 65-mmHg intraventricular gradient. After the 110-mmHg extrasystole bubble contrast was injected to choose the target septal branch (figure 3) followed by the injection of 0.1 mL of alcohol per millimeter of contrasted septum. In the echocardiography a 23 mm contrasted septum was measured, and 2.3 mL of alcohol were administered in the second septal branch.
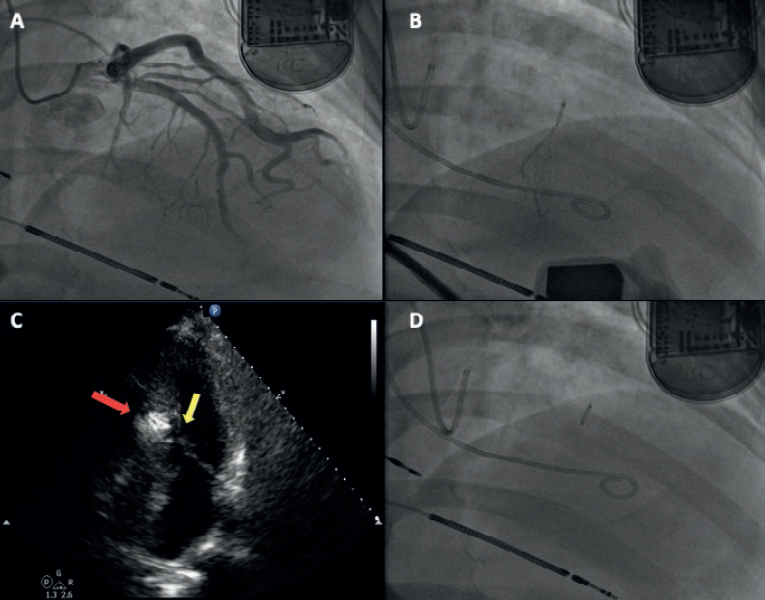
Figure 3. A: coronary angiography. B: injection of bubble contrast in the second septal branch. C: contrast enhancement of the susceptible septal region (arrow). D: over-the-wire balloon used for the administration of alcohol.
SUPPLEMENTARY DATA
Video 1. Custodio-Sánchez P. DOI:10.24875/RECICE.M19000070
Corresponding author: Juan Badiano 1, Col. Belisario Domínguez, Sección XVI, 14080 Tlalpan, Mexico City, Mexico.
E-mail address: custodiomed@hotmail.com (P. Custodio-Sánchez).











